ABSTRACT
As the elderly population continues to grow and strains public medical finances, there is a pressing need for innovative solutions to address the impending exhaustion of resources for elderly care. One such solution is the concept of community care, which offers an alternative approach to traditional elderly care services. However, limited research has explored the effectiveness of community care in situations where elderly care services are inadequately provided due to a shortage of care facilities in rural areas. In this study, we propose a framework known as "Community Care for Rural Seniors" to address the challenge of under-provisioned elderly care in rural communities. Our approach centers on the development of caring communities, comprised of local residents, as the primary providers of elderly care in rural settings. These caring communities establish and manage essential elderly daycare centers and facilities, ensuring a more comprehensive elderly care service infrastructure in rural areas. To ensure the sustainability of these caring communities, we recommend that both central and local governments provide support and resources. This collaborative effort can foster the growth and longevity of community care for rural seniors, offering a viable solution to the challenges posed by the shortage of elderly care facilities in rural regions.
Keywords: community care, caring community, elderly care, care delivery system
INTRODUCTION
According to Statistics Korea, the aging rate in Korea was 14.8% as of 2018, an increase of 3.31% from 2010 (Statistics Korea, 2019a). Accordingly, Korea entered the aged society in 2018, 18 years after entering the aging society in 2000, and will enter the super-aged society in 2025. The proportion of elderly people living alone is also high. The proportion of elderly people living alone in South Korea was 19.5% in 2019, up by 3.5% from 16.0% in 2000 (Statistics Korea, 2019b). The proportion of single-person households among the elderly is also high at 34.2%. Without family members living with them, the elderly people living alone are more likely to feel abandoned and lonely, and are less likely to receive timely care in the event of an emergency.
As the population ages and the number of elderly people living alone increases, how to care for the elderly has become an important issue. In Korea, families have traditionally been responsible for the care of the elderly, but as the elderly population has grown and extended families have disintegrated, care facilities have taken over. As a result, the number of elderly care facilities in Korea increased from 1,642 in 2009 to 3,390 in 2018, and the capacity of the facilities increased from 82,271 to 160,594 (Ministry of Health and Welfare, 2019a). The number of nursing homes also increased from 777 in 2009 to 1,558 in 2018, and the number of licensed beds increased from 90,144 in 2009 to 301,296 in 2018 (National Health Insurance Service, 2019).
However, it is questionable whether elderly people in nursing homes are able to lead healthy daily lives. Since the number of residents determines the profitability of the facility, it is common for facilities to operate with the goal of maximizing profits. Therefore, it is known that hygiene and nutrition are often neglected in order to save on operating costs.
An aging population poses a huge problem for healthcare financing. As of 2018, the average number of days spent in a nursing facility in the 10 years before death for people aged 65 and older was 707 days. Medical and nursing care expenses for the elderly totaled US$5.1 billion in the 10 years before their deaths, or about US$38,600 per person. Of this amount, US$4.3 billion was covered by the National Health Insurance Service, or about US$32,000 per person (National Health Insurance Service, 2019). The problem of medical expenses for the elderly is also serious. In 2018, medical expenses for the elderly aged 65 and over, who make up 14% of the total population, accounted for 40.8% of total medical expenses (Health Insurance Review and Assessment Service et al., 2019).
The Ministry of Health and Welfare is promoting community integrated care (hereinafter referred to as community care) as a policy alternative to health and welfare services in order to respond to the human rights issues in facilities and the depletion of healthcare finances due to the aging population. It defines community care as "an innovative social service system that aims to enable residents in need of care to live in the community, such as at home or in a group home, enjoy welfare benefits and services tailored to their individual needs, live together with the community, and engage in self-actualization and activities" (Ministry of Health and Welfare, 2018b). It provides health care services such as medical treatment and nursing care, as well as care services to help with daily living activities, in an integrated manner within the community, centered on the needs of the person served. It aims to support people to live their lives in their familiar homes and communities. Accordingly, the Ministry announced the “Community Care Pilot Project” and selected local governments for the project. (Ministry of Health and Welfare, 2019b).
However, rural areas are different from urban areas, and it is difficult to apply the pilot project model to rural areas because the target population in rural areas hardly access medical and care facilities. Currently, the pilot project focuses on expanding home health care and home visits to medical institutions such as hospitals and care providers such as welfare centers, and providing integrated health and care services. The problem is that rural areas lack access to healthcare and care-related infrastructure and have fewer care and healthcare workers. The Community Care Pilot Project proposes the following strategies for integrating healthcare and care: chronic disease management in residential support and nursing care, promoting home visits, intensive healthcare, home-based long-term care services, and customized rehabilitation, but rural areas are a difficult environment to implement these strategies.
The purpose of this study is to propose a community care promotion system suitable for rural environments. By analyzing the care supply and demand system in rural areas and identifying available human and material resources and possible projects, we propose a direction for community care projects led by rural residents.
Also, a system for rural residents is provided to take the lead in community care. In response to the shortage of caregivers and supply systems in rural areas, this study proposes a promotion system for residents to take the initiative in planning and participating in care. In rural areas where there is a critical shortage of care or healthcare support facilities and personnel, present a participatory framework for rural residents who are potential care providers to take an active role in community care in their area.
This study also suggests a system for linking communities, local governments, agricultural activities, and agribusiness to provide integrated care. It analyzes the possibility of linking case finding, needs assessment, care, and health care services that have been implemented by different organizations. Rather than presenting a one-size-fits-all model, this study suggests ways for various actors to work together as a caring community.
The primary focus of the study is rural seniors. Community care targets all vulnerable populations in need of care in the community, including the elderly, mentally ill, disabled, and homeless. However, given the aging rate and lack of care delivery systems in rural areas, this study focuses on the elderly and draws implications for the community care promotion system.
ELDERLY CARE SYSTEMS IN SOUTH KOREA
Overview of elderly care systems
The main public elderly care services in Korea are the Long-Term Care Insurance and Elderly Personalized Care Services. According to Article 1 of the Long-Term Care Act, the Long-Term Care Insurance is a social insurance system that provides long-term care benefits such as support for physical activities and household activities to the elderly who are unable to perform daily activities alone due to reasons such as old age or senile diseases, with the purpose of improving the quality of life of the elderly by promoting their health and stabilizing their lives and reducing the burden on their families. It aims to reduce the financial burden of care for the elderly in order to promote their health and stability in their later years.
The most important feature of the Long-Term Care Insurance system is its universality. It operates as a universal care system that considers the physical and cognitive functioning status of the elderly, regardless of their income, determines a rating, and provides services according to the rating. It identifies the care needs of the entire elderly population and provides services that meet the needs of each individual.
Another feature of the system is that most organizations for providing care services under the Long-Term Care Insurance are private. The National Health Insurance Service manages and operates the system, using premiums paid by the insurance subscribers and government subsidies. However, the organizations or facilities providing care are not public institutions, but private facilities established under the Elderly Welfare Act. Therefore, it is difficult to ensure sufficient supply in places where absolute demand is low and profitability is lacking, such as rural areas.
The Elderly Personalized Care Services is a care service provided by local governments that provides care for the elderly who have difficulty in performing daily activities but are not eligible for the Long-Term Care Insurance. It aims to ensure a stable old age and maintain the health and physical function of the elderly, preventing them from entering high-cost care services such as the Long-Term Care Insurance.
The Elderly Personalized Care Service is an optional care system and not all elderly people are eligible for the service. Service recipients must not be eligible for similar programs, such as those aged 65 or older who receive the National Basic Livelihood Program and the next higher tier, or those who receive the Basic Pension Program and are eligible for the Long-Term Care Insurance. For example, elderly people who need care, such as elderly people living alone, grandparents, or elderly households, or elderly people who suffer from physical decline, cognitive decline, depression, or are at high risk of loneliness or suicide, must meet certain income standards.
DEMAND FOR RURAL ELDERLY CARE
According to Table 1, it is estimated that about 1.95 million elderly people, or 24.3% of the 8.03 million elderly people aged 65 and over in Korea, are potential care seekers who have difficulty leading their daily lives. Based on the Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL), 74.7% of the elderly have no functional limitations, leaving 25.3% who need care.
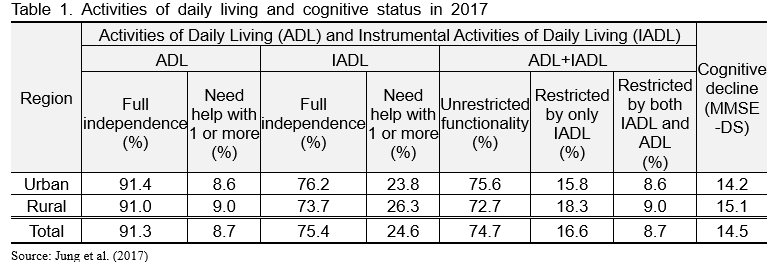
Of the 1.95 million potential care seekers, we estimate that about 1.12 million are receiving public care, leaving 795,000 in the care gap. As of the end of 2019, there were 765,000 elderly people in the group receiving the Long-Term Care Insurance benefits plus 350,000 people receiving the Elderly Personalized Care Services. The total number of seniors who take the public care is about 1.12 million, or 13.8% of the total elderly and 57.2% of the elderly with potential care needs. Assuming that 30% of the elderly population aged 65 and over live in rural areas, about 240,000 elderly people do not have the chance to take the public care services.
LIMITATIONS OF RURAL ELDERLY CARE SUPPLY
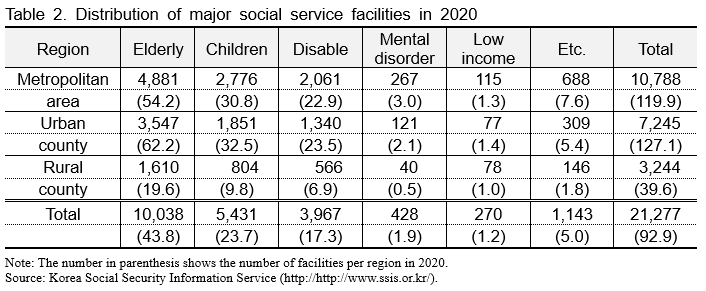
The biggest problem with the care supply system in rural areas is that facilities to provide care are concentrated in cities, and rural residents' access to facilities is significantly more difficult than that in cities. As shown in Table 2, there are an average of 54.2 elderly welfare facilities per metropolitan areas, but only 19.6 in rural county areas. Social welfare facilities, including elderly welfare facilities, are also mainly located in cities, with an average of 119.9 facilities per urban cities, but only 39.6 facilities per rural town. Therefore, rural residents have to travel farther than urban seniors to access services.
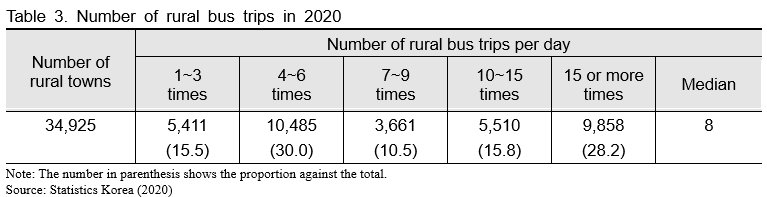
Poor transportation in rural areas is also a problem. It is difficult to imagine residents with health problems traveling to care facilities by car. According to Table 3, the average number of bus trips per town per day is only 6.1, with 20 percent of the regions having fewer than three bus trips per day or no bus trips at all. The same is true for taxis, another form of public transportation. Furthermore, 78.8% of all counties have two or fewer taxis on standby. Therefore, it is virtually impossible for people living at the village level to access care facilities located in the center of a town or county in a timely manner.
COMMUNITY CARE THEORY AND PROGRAM PRACTICE
The Multidimensionality of Community Care
Community care should fulfill the following two premises. The first is that the care recipient moves from an isolated facility to the community and provides integrated care from service planning to care centered on the needs of the care recipient. The second is that the care recipient is not isolated in the community but lives as a member of the community, meaning that the care recipient participates in community activities and the community recognizes the vulnerable as a member of the community.
From this perspective, community care can be defined based on the multidimensionality of 'community' and 'care' as shown in Table 4. Community is defined in terms of three dimensions: "community as a space (in the community)," "devolution of power to localities (decentralized community)," and "community as an active subject (by the community)," and care is defined in terms of three dimensions: " medical & health care," " long-term & social care," and "social inclusion " (Kim, 2018a, 2018b).
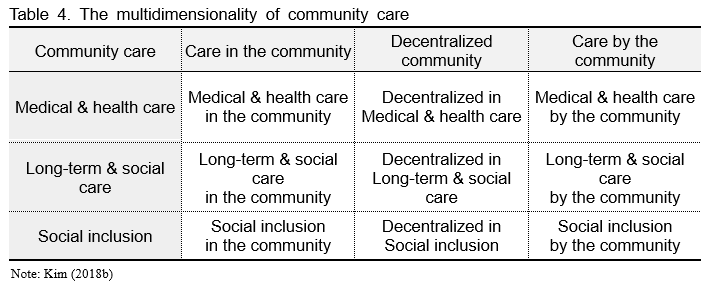
Community as a space is deinstitutionalization. It involves moving people from institutions to the community and attempts to prevent social hospitalization, where a lack of care leads to institutionalization. It allows the community to provide care based on the person's needs, rather than forcing them to live in an institution that ignores their diverse needs.
Devolution of power to the local level means that local governments actually play an active role in planning and strategizing community care projects. It ensures that local governments have the responsibility and authority for the overall care, so that they can implement community-based care based on the needs of the recipients. Reasonable division of roles between the central government and local governments, with local governments taking responsibility for providing community-based care in partnership with the private sector.
Communities as actors is based on communities and residents taking the lead in planning and providing care, rather than having care provided by the central government or local governments. In conventional care, the government provides one-size-fits-all care and the person receiving care is not involved in the planning or delivery of care. However, community-driven care provides opportunities for not only care providers but also care recipients to participate in care to restore and revitalize their communities.
Care includes three dimensions: health care, nursing and care services, and social inclusion. Health and medical services are services such as medical treatment, nursing care, and rehabilitation provided by medical institutions under the National Health Insurance System to care recipients. Nursing and care services refer to integrated services such as housekeeping, care, nursing, and rehabilitation provided by facilities for the elderly or people with disabilities and focus on providing a variety of daily living support services. Social inclusion means supporting people in care to become part of the community by participating in jobs, leisure and sports activities, community activities, etc. in addition to direct health and medical services and nursing and care services.
CURRENT STATUS OF COMMUNITY CARE PILOT PROJECT
The pilot project was conducted nationwide in two rounds with local governments. A total of eight local governments were selected for the first round, including four models of integrated community care for the elderly, two models of independent living and community settlement for the disabled, and one model of community settlement support for the mentally ill. For the second round, two metropolitan areas, one rapidly aging area, three urban-rural complexes, and two rural areas were selected to cover a wide range of localities according to local characteristics.
The pilot project seems to focus on "deinstitutionalization" to realize community as a space. It sends care recipients currently in facilities to the community and supports them to settle and live in the community. To help those who have been discharged live in the community, residential support infrastructure is expanded, and home healthcare and home care services are provided. For example, projects targeting the elderly provide integrated medical care, and needs assessments to elderly people who have been admitted to a nursing hospital or nursing home to help them return to the community. It is aimed at elderly people who are preparing to be discharged from nursing facilities and elderly people who live in the community but are unable to enter a facility due to difficulties in their daily lives. Local governments will conduct a needs assessment and develop an individualized support plan, including a discharge plan. The hospital's local coordination office will develop a discharge plan and connect with care information centers. Home repair, home medical care, and in-home services will be provided to help the elderly with limited mobility live comfortably at home. It also emphasizes the establishment of community health centers to provide health care and comprehensive rehabilitation centers to expand long-term care at home.
Another feature of the pilot project is that it emphasizes the devolution of power to local governments, allowing them to plan and operate necessary services with autonomy. For example, city and district community care councils are responsible for selecting community care recipients, coordinating and discussing individual cases, and finalizing and implementing integrated care plans, while city, county, and district convergence service teams support the operation of community care councils. Town, village, and district care information centers provide comprehensive counseling, reception, application, and follow-up checks and inspections. Local governments at the county level have been given the authority to carry out care-related planning and financial execution, allowing local governments to carry out projects that were previously planned and operated by the central government.
However, there are limitations to implementing the project in rural areas. First of all, policies that focus on deinstitutionalization in rural areas are not effective. This is because the probability that a person discharged from a facility will settle in a rural area is extremely small. For example, if a person is admitted to a nursing home in a county, their original residence is likely to be in an urban area. the probability of returning to the rural area after discharge is extremely low because they want to live their original residence, but not rural area where they temporarily resided. This is why services targeting institutionalized persons in rural municipalities are unlikely to be effective.
There is also a problem with the emphasis on building and improving care facilities rather than the original purpose of providing welfare benefits that meet individual needs. Installing facilities in rural areas where care is scarce is positive. However, it is difficult to establish such facilities in villages with low population density, where there is neither economic benefit nor absolute demand to ensure minimum efficiency. It is clear that most of the new facilities will be located in municipal centers, and the beneficiaries of facility improvement projects are likely to be centrally located facilities. Therefore, it is difficult to establish new care facilities in rural areas, and it is difficult to attempt to improve existing facilities.
The role of local communities as drivers was also overlooked. Some of the local governments selected for the first round of pilot projects proposed using village communities or social economy organizations to provide integrated care or to match volunteers with clients. However, not only is it unclear how these plans will be implemented, but rural areas are also vulnerable to hiring people to work in social and economic organizations or finding volunteers. While this can be considered as a short-term solution, it is unlikely to be sustainable in the future without an organized workforce and decent wages.
The care recipients were also thoroughly neglected. In community-based care, trust and cooperation between caregivers and care recipients are important. However, none of the pilot municipalities had planned any organizations or projects that directly involved the recipients. Unlike cities, rural areas are characterized by local community traditions. A community care model that pursues the community as a space and the community as a subject can be completed if it is led by the local community, where care providers and care recipients coexist in accordance with the traditions of the local community. The top-down project promotion led by local governments has also excluded the role of the community as a care provider.
POLICY DIRECTION OF RURAL COMMUNITY CARE
Overview
To overcome the limitations of rural areas in the elderly care system, rural community care should be primarily community-driven. The community should be at the center of the role in providing care and overcoming the limitations of rural resources and access to resources. Conflicts between providers and recipients should be mediated within the community, and local people should be empowered to plan and organize the services they need and how they are delivered. We need to move away from the role of providing care within the public care system to one that is inclusive of all people in the community and restores a sense of community in rural areas. In rural areas where there is a history of cooperation and solidarity among local communities, community-led care can be an alternative way of addressing the challenges of rural care systems.
Based on the perspective that the community becomes the subject of care, we will discuss the direction of promoting rural community care. We would like to suggest the direction that rural community care should pursue in terms of targets, promoters, how to discover cases, how to provide care and set up facilities, and how to link with other projects.
Eligibility
The physical and cognitive functioning status of the elderly can be categorized into four main categories based on the classification of the Long-Term Care Insurance and the classification criteria for the home health care project. 'Healthy seniors' are seniors who are able to perform daily activities and have no mental or psychological problems, 'potentially ill seniors' are seniors who do not have major problems with daily activities but are experiencing some discomfort and are likely to experience a decline in physical function or cognitive status in the future, 'lightly ill seniors' are seniors who have begun to experience a decline in functional status and require simple care, and 'severely ill seniors' are seniors who are unable to perform daily activities and require full care.
The Long-Term Care Insurance provides care for seniors in critical condition. Elderly people with severe conditions are in tier 1 or 2 of the insurance and can be admitted to a nursing home or nursing hospital. Lightly ill elderly people are cared for in a home-based elderly welfare facility with levels 3-5 of the Long-Term Care Insurance. As mentioned earlier, about 765,000 elderly people receive benefits and can be cared for in long-term care facilities in rural areas.
The Long-Term Care Services are available in rural areas, but rural seniors do not have sufficient access to long-term care services, especially day care. According to elderly care experts and activists, every community with a population of 2,000 or more, or an elderly population of 700 or more, must have at least one day care center. Day care centers provide a variety of physical and social programs for those eligible for the Long-Term Care Insurance and help seniors maintain social connections. However, 67.8% of all counties in Korea and 61.9% of counties with 700 or more elderly people do not have day care centers under the Elderly Welfare Act or the Long-Term Care Act.
About 735,000 elderly people with mild conditions are eligible for personalized care services, but they are unable to receive care. In particular, about 30% of those eligible for the service live in towns and villages, so it is likely that at least 200,000 people are potentially eligible for the service but do not receive proper care. Moreover, the government has budgeted US$288.1 million for the elderly personalized care service, which is only about KRW100 million per town and village and about KRW200,000 per potential recipient. This is not enough to provide sufficient services in rural areas.
Rural community care is intended for rural elderly adults who are underserved due to a lack of long-term care and aging-in-place services, and for rural seniors who are currently healthy but are likely to decline in physical function or cognitive status in the future. Rural community care complements the aged care delivery system in rural areas and provides preventive care to prevent potential eligible from developing mild or severe conditions.
Drivers
The community care currently being discussed lacks a channel to realize the community as a subject. The Ministry of Health and Welfare's community care pilot project is led by local governments, but the problem is that local governments are not communities. In the pilot project, the local government's care center or service team is responsible for establishing the community care system and planning and coordinating the project. It is appropriate for local governments to discover and verify pioneering project models and create localized models in terms of decentralizing care. However, it is difficult for community care led by municipalities to reach rural areas at the village level, which are spatially distant.
Rural community care should be driven by residents. Local care needs are best understood by the people who have lived in the area for the longest time and by the people who are the recipients. For example, suppose there is an elderly person in your village who is not eligible for the Long-Term Care Insurance or personalized care services for the elderly, but would like a bath or lunch delivery service. If the elderly person does not actively express their needs, it is difficult to provide the service. It is difficult for municipalities and community centers that are spatially distant from the village to actively seek out and serve this person. Residents who live and interact with their neighbors are best suited to identify and connect them to public care.
To implement resident-led community care projects, you need a local community organization. Typically, these organizations include only a few recognizable residents, such as the head of the village or the village treasurer, but it is important for residents of all backgrounds to participate in community care projects. This is because the community is only sustainable if everyone agrees on the purpose and direction of the community. However, it is rare for a voluntary organization to form spontaneously in a short period of time. In fact, the Ministry of Health and Welfare's community care pilot project has a two-year duration, and after one year, care facilities have been created, but none of them are led by resident organizations. Therefore, we need to think about how to organize communities to ensure residents' participation and enable efficient community care projects.
Discovering care cases
One of the keys to community care is to identify the needs of the recipients and provide care based on their needs. In order to identify the needs of the recipients, it is necessary to discover recipients with care needs, and in the integrated care pioneering project, the care information desks of town, village, and community centers play a role. Among the cases discovered by the care information centers, those that can be managed within the town and village are solved by themselves, and those that are difficult to solve are provided with care in conjunction with the local care council of the city and district.
The problem is that it is difficult for town and village care information centers to discover cases and potential beneficiaries. The pilot project places one or two community care counselors at the community center. However, it is difficult for one or two counselors to find people who live in large areas such as towns and villages. They cannot help providing services unless the person comes to the care information center.
Rural community care puts residents in the role of connecting people with care services. Residents know their area and neighbors best and have no problem accessing clients. Local people can identify people in need and connect them with local government outreach workers or case managers. Connecting with local neighborhood councils, such as Community Security Councils, whose purpose is to identify welfare blind spots in the community can make case finding more efficient.
Provision of care
Providing care to eligible people at the village level requires setting up a care facility within the village or setting up a facility in a district center and providing transportation. Private for-profit care facilities are difficult to establish in rural areas because the absolute demand is not high enough to make it profitable. In rural villages, there are also senior centers, which are leisure welfare facilities for the elderly. However, it is difficult to call it a care facility as it only requires a space of 20 m2 or more that can be used by more than 20 people (10 people in towns and villages).
Rural community care is a system in which residents plan and provide care directly or indirectly. To provide the Long-Term Care Insurance services for the elderly or customized care services for the elderly, caregivers and support workers are needed. Villages and districts can provide care themselves if they have residents who can perform the duties of a caregiver or support worker. You can also support training courses to help them become qualified. The care needed for potentially elderly people is day-to-day care that doesn't require specialized knowledge. This type of care, such as checking in on neighbors or identifying and connecting with neighbors in need, has a long history in rural communities. More specialized care can be provided by residents who have received some education or training or are caregivers.
Rural community care focuses on the relational nature of care. Care is based on the mutual recognition of caregivers and recipients, and the quality of care is enhanced when providers and recipients work together based on trust and cooperation (Kim 2015). Care is a co-production in the sense that the quality of care is determined by the relationship between the care provider and the care recipient. From the perspective of co-production, professionals should not assess the needs of users and develop services, but users should participate as active agents who express their own needs and lead the development of services. The effectiveness of care is also higher when care is provided by a resident who understands their current condition than by someone who does not know them at all. When care is planned and delivered by people who are not currently eligible but may become eligible in the future, it is more likely to be the most appropriate and necessary care for them.
Residents who participate in care should be paid a fair price for their labor. Rural residents are primarily engaged in agriculture and cannot stop farming to provide care. If you don't compensate them for the opportunity cost of providing care, the care they provide will not be sustainable. Therefore, if they spend part of their farming time providing care, you should compensate them or hire them for part-time work or a second job.
Medical personnel, such as nurses, are needed to promote the health of the target population and manage chronic diseases. In rural areas, one organization that can play this role is a health center. Health clinics are the smallest level of public healthcare, staffed by public health officials who are nurses and hold a nursing license, according to the Special Measures for Healthcare in Rural Areas Act. There are 1,904 clinics nationwide, with each clinic covering 5-10 villages, providing good access to the target population. Medical consumer life cooperatives (hereinafter referred to as medical cooperatives) that operate in rural areas are also an alternative. However, there are difficulties with the establishment standards that do not match the reality of underdeveloped rural areas, and the system needs to be improved.
Establishment of care facilities
Rural community care projects require two types of facilities: central care facilities that provide specialized care, such as day care centers, and small village care facilities that provide the physical and emotional support needed to lead a normal life, such as assisted living, daily care, and emotional care.
It is unlikely that care facilities will be paid for by the community. A viable alternative is to utilize central government or local government community development programs, especially the Ministry of Agriculture's General Rural Development Program. The purpose of the program is to restore rural livelihoods and strengthen connections between centers by expanding investments in poor rural infrastructure. This is consistent with the goal of rural community care, which is to restore local welfare communities by expanding care infrastructure in rural areas. Under this project, facilities such as day care centers can be established in rural centers through the various project conducted in rural areas.
A day care center can be established in the center of the rural town. As mentioned earlier, there must be at least one day care center in every county that provides long-term care services. Despite this urgency, about 60-70% of all rural towns in South Korea do not have day care centers. By utilizing the development project mentioned above, a day care center can be established in the center of the county to provide high access to day care for the elderly.
Along with day care centers, care centers will be established to support rural community care. The care support center will be home to the secretariat that plans and manages community care, performing tasks such as planning care provision, operating day care facilities and village care facilities, linking with local care organizations, and researching and utilizing local physical and human resources. Providing the secretariat with a location for its activities ensures that rural community care projects are carried out efficiently.
Small-scale care facilities can be set up by improving the existing senior centers at the village level. As of the end of 2018, there were about 66,286 senior centers nationwide, many in rural areas, and they play an important role in the welfare service delivery system. However, due to their small facilities and lack of specialized staff, they only play a role in building relationships and communication within the community. Improving the facilities of these rural senior centers can help reduce the cost of building care facilities and ensure accessibility to the target population.
Transportation to care facilities can also be provided. To visit the day care center in the center of the village, transportation is needed, and the problem of transportation can be solved by using the center revitalization project, the basic living base project, and the rural transportation model visit project. Introduce a "village care bus" so that villagers can visit day care centers in the center of the county.
Linking projects
For a rural community care project to be successful, community participation is essential. If the administration plans and operates from the top down, projects that ignore the actual needs of local residents will be created, and the sustainability of the project will be lost, resulting in idle facilities and operating costs. Therefore, it is necessary to identify local resources and make plans to link various projects through direct participation of residents.
The project of establishing and implementing a resident-led village welfare plan can be used in the rural community care planning stage. Village welfare planning is a project in which towns and villages develop and implement plans for small-scale agendas that can be solved on their own, such as neighbor care and community welfare schools. Engage residents and provide educational programs so that they can actually participate.
If you have a neighborhood association, you can also utilize the neighborhood plan. In the community self-governance plan, residents participate to organize subcommittees, discover village agendas, and establish self-governance plans for each subcommittee. The welfare division can plan rural community care projects and establish mid- to long-term action plans for public discussion.
At the implementation level, it can be linked to social farming. Social farming is defined as "agricultural practices that bring the socially excluded into society" (Kim 2017), meaning agricultural activities that provide care, education, and employment to vulnerable rural populations, such as those without jobs, those with mental and physical disabilities, and those who want to learn agriculture, for the purpose of rehabilitation and self-reliance. Rural community care targets include the elderly and the chronically mentally disabled who are not cared for by the public care system. Therefore, social farming can be recognized, connected, and provided as a form of care.
The reason why social farming is effective as care is that agricultural activities are the most familiar activities in rural areas. The target audience are the rural residents. They have a lot of experiences with agricultural activities and social interactions, so they can easily adapt. Social farms are also easy to access because they are located in rural areas. Instead of having to travel to the center of town for occupational therapy, they can participate in social farming programs offered by their neighbors. In fact, the social farms selected for the 2020 Social Farming Revitalization Support Project provide social farming programs for the underprivileged in rural areas, such as people with dementia, people living alone, people with disabilities, farmers and villagers, and young farmers. Collaborating with neighboring social farms provides an opportunity to improve the effectiveness of community care.
CONCLUSION AND FUTURE CHALLENGES
The key to rural community care is that it is driven by local communities, not institutions. It centers on the community and provides care to those who do not receive sufficient care in the existing care delivery system, or who need preventive care but do not receive public care benefits. Plan care from the perspective of the care recipient and provide care to their neighbors. Coordinate with other community organizations and local governments to provide efficient care. It is the role of the caring community to strive to provide diverse and effective care by installing and operating care facilities and providing social farming programs in conjunction with agricultural businesses.
Support caring communities to create a secretariat to run rural community care. A top-down system of care is possible when caring communities are supported to create a secretariat to run community care. Because caring communities are organized by residents, they need to organize and set up a secretariat with expertise. The secretariat can perform a variety of tasks, including conducting needs assessments, running and evaluating facilities, and engaging and collaborating with the community. These tasks need to be carried out with professionalism and continuity, which requires a full-time person in the secretariat and adequate compensation for the full-time person. Therefore, the caring community should be supported by the central government or local government in hiring and running the secretariat staff.
Rural community care is a bottom-up system of care. Rather than central government or local governments planning and delivering care, it is a system that supports communities of people to plan and run their own care. In the early stages of the project, community learning organizations and the communities they organize will be supported in a phased manner. Support the learning organization to identify care needs in the village and create a care plan that considers the local context. Then, once the learning organization is transformed into a community care organization, we provide subsidies to help them set up and operate care facilities and pay for care workers. Only by operating from the bottom up can community care become a sustainable rural care delivery system.
From this point of view, a social economic organization, in particular a social cooperative, may be the most appropriate legal entity for the community. When a community becomes a social cooperative, care recipients and providers can operate in the same community in cooperation and solidarity for the purpose of providing care based on co-production (Cho 2014), and both recipients and providers can participate in the management of the community as subjects, ensuring the sustainability of the community. Therefore, social cooperatives can be an alternative way to lead rural community care.
In conclusion, rural community care is defined as "a system in which a caring community, a resident care organization, with the participation of all residents, utilizes existing human and physical resources and subsidized projects provided by the government to provide preventive care to the recipients and include the recipients in the community". It is a system in which resident community organizations plan projects with the central government and local governments and use a combination of internal and external physical and human resources to provide professional care, daily support, health promotion programs, and chronic disease management.
Future research challenges include First, the actual needs of rural elderly people should be investigated and services should be planned. It is necessary to investigate the actual care needs of rural elderly people and plan service provision accordingly, such as entering facilities such as nursing homes, expanding the Long-Term Care Insurance and elderly-specific care services, establishing day care centers, providing home-based care and daily care, expanding health-related programs per elderly person, and increasing community activities.
Caring communities should be provided with specific information about what they need to do to implement rural community care. If there are local residents who are interested in rural community care, they should be provided with accurate information in order to provide services. In particular, specialized information such as how to set up and operate a care facility and the care delivery system should be provided. For example, you should provide specific information on the actual cost of the care facility, the hiring of staff, the legal status of the operating entity, and the utilization of subsidized projects. Only when communities have this information can they plan and operate their care provision, reducing the risk of failure and increasing the likelihood of success.
Finally, rural communities need to be mindful of central government programs and ensure that they can continue even if funding is cut off. Care in rural areas is particularly difficult to monetize, making it unlikely that private organizations or facilities will be able to enter the market. Therefore, care support projects implemented by the Ministry of Health and Welfare or local governments should be coordinated. For example, rural community care can be provided with support from the Ministry of Health and Welfare or local governments, including care for the severely ill. Sustainability issues should be considered not only by the Ministry of Health and Welfare, but also by the Ministry of Agriculture.
REFERENCES
Cho, M. (2014). Feasibility Exploration of Social Cooperatives as a Community Social Work Practice Model. Journal of Agricultural Extension & Community Development, 21(3), 91-119.
Health Insurance Review and Assessment Service. (2019). Health Insurance Statistical Year Book.
Jung, K., Oh, Y., Lee, Y., Oh, M., Kang, E., Kim, K., Hwang, N., Kim, S., Lee S., Lee, S., & Hong, S. (2017) Survey on the Elderly. Korea Institute for Health and Social Affairs.
Kim, E. (2015). A community approach for establishing the effective social care system. Korean Journal of Social Welfare Studies, 46(2), 153-176.
Kim, J., An, S., Lee, J., & Kim, K. (2017). Social Farming in Rural Korea and Policy Direction. Korea Rural Economic Institute. 1-121.
Kim, Y. (2018a). Deinstitutionalization and Building Community-Based Personal Social Services: Community Care that Connects Independence and Interdependence. Health and Social Welfare Review, 38(3), 492-520.
Kim, Y. (2018b). Community care, what to do and how to do it? Welfare Trend, 238, 5-10.
Ministry of Health and Welfare. (2019a). 2019 Status of Welfare Facilities for the Elderly
Ministry of Health and Welfare. (2019b). Community Integrated Care (Community Care) Pilot Project initiative.
National Health Insurance Service. (2018). Long Term Care Insurance Statistical Year Book.
National Health Insurance Service. (2019). Average length of stay in nursing homes and assisted living facilities by state for persons aged 65 and older in 2018.
Statistics Korea. (2020). 2020 Census of Agriculture, Forestry and Fisheries.
Statistics Korea. (2019a). 2018 Population and Housing Census.
Statistics Korea. (2019b). Statistics for seniors.


Community Care for Rural Seniors
ABSTRACT
As the elderly population continues to grow and strains public medical finances, there is a pressing need for innovative solutions to address the impending exhaustion of resources for elderly care. One such solution is the concept of community care, which offers an alternative approach to traditional elderly care services. However, limited research has explored the effectiveness of community care in situations where elderly care services are inadequately provided due to a shortage of care facilities in rural areas. In this study, we propose a framework known as "Community Care for Rural Seniors" to address the challenge of under-provisioned elderly care in rural communities. Our approach centers on the development of caring communities, comprised of local residents, as the primary providers of elderly care in rural settings. These caring communities establish and manage essential elderly daycare centers and facilities, ensuring a more comprehensive elderly care service infrastructure in rural areas. To ensure the sustainability of these caring communities, we recommend that both central and local governments provide support and resources. This collaborative effort can foster the growth and longevity of community care for rural seniors, offering a viable solution to the challenges posed by the shortage of elderly care facilities in rural regions.
Keywords: community care, caring community, elderly care, care delivery system
INTRODUCTION
According to Statistics Korea, the aging rate in Korea was 14.8% as of 2018, an increase of 3.31% from 2010 (Statistics Korea, 2019a). Accordingly, Korea entered the aged society in 2018, 18 years after entering the aging society in 2000, and will enter the super-aged society in 2025. The proportion of elderly people living alone is also high. The proportion of elderly people living alone in South Korea was 19.5% in 2019, up by 3.5% from 16.0% in 2000 (Statistics Korea, 2019b). The proportion of single-person households among the elderly is also high at 34.2%. Without family members living with them, the elderly people living alone are more likely to feel abandoned and lonely, and are less likely to receive timely care in the event of an emergency.
As the population ages and the number of elderly people living alone increases, how to care for the elderly has become an important issue. In Korea, families have traditionally been responsible for the care of the elderly, but as the elderly population has grown and extended families have disintegrated, care facilities have taken over. As a result, the number of elderly care facilities in Korea increased from 1,642 in 2009 to 3,390 in 2018, and the capacity of the facilities increased from 82,271 to 160,594 (Ministry of Health and Welfare, 2019a). The number of nursing homes also increased from 777 in 2009 to 1,558 in 2018, and the number of licensed beds increased from 90,144 in 2009 to 301,296 in 2018 (National Health Insurance Service, 2019).
However, it is questionable whether elderly people in nursing homes are able to lead healthy daily lives. Since the number of residents determines the profitability of the facility, it is common for facilities to operate with the goal of maximizing profits. Therefore, it is known that hygiene and nutrition are often neglected in order to save on operating costs.
An aging population poses a huge problem for healthcare financing. As of 2018, the average number of days spent in a nursing facility in the 10 years before death for people aged 65 and older was 707 days. Medical and nursing care expenses for the elderly totaled US$5.1 billion in the 10 years before their deaths, or about US$38,600 per person. Of this amount, US$4.3 billion was covered by the National Health Insurance Service, or about US$32,000 per person (National Health Insurance Service, 2019). The problem of medical expenses for the elderly is also serious. In 2018, medical expenses for the elderly aged 65 and over, who make up 14% of the total population, accounted for 40.8% of total medical expenses (Health Insurance Review and Assessment Service et al., 2019).
The Ministry of Health and Welfare is promoting community integrated care (hereinafter referred to as community care) as a policy alternative to health and welfare services in order to respond to the human rights issues in facilities and the depletion of healthcare finances due to the aging population. It defines community care as "an innovative social service system that aims to enable residents in need of care to live in the community, such as at home or in a group home, enjoy welfare benefits and services tailored to their individual needs, live together with the community, and engage in self-actualization and activities" (Ministry of Health and Welfare, 2018b). It provides health care services such as medical treatment and nursing care, as well as care services to help with daily living activities, in an integrated manner within the community, centered on the needs of the person served. It aims to support people to live their lives in their familiar homes and communities. Accordingly, the Ministry announced the “Community Care Pilot Project” and selected local governments for the project. (Ministry of Health and Welfare, 2019b).
However, rural areas are different from urban areas, and it is difficult to apply the pilot project model to rural areas because the target population in rural areas hardly access medical and care facilities. Currently, the pilot project focuses on expanding home health care and home visits to medical institutions such as hospitals and care providers such as welfare centers, and providing integrated health and care services. The problem is that rural areas lack access to healthcare and care-related infrastructure and have fewer care and healthcare workers. The Community Care Pilot Project proposes the following strategies for integrating healthcare and care: chronic disease management in residential support and nursing care, promoting home visits, intensive healthcare, home-based long-term care services, and customized rehabilitation, but rural areas are a difficult environment to implement these strategies.
The purpose of this study is to propose a community care promotion system suitable for rural environments. By analyzing the care supply and demand system in rural areas and identifying available human and material resources and possible projects, we propose a direction for community care projects led by rural residents.
Also, a system for rural residents is provided to take the lead in community care. In response to the shortage of caregivers and supply systems in rural areas, this study proposes a promotion system for residents to take the initiative in planning and participating in care. In rural areas where there is a critical shortage of care or healthcare support facilities and personnel, present a participatory framework for rural residents who are potential care providers to take an active role in community care in their area.
This study also suggests a system for linking communities, local governments, agricultural activities, and agribusiness to provide integrated care. It analyzes the possibility of linking case finding, needs assessment, care, and health care services that have been implemented by different organizations. Rather than presenting a one-size-fits-all model, this study suggests ways for various actors to work together as a caring community.
The primary focus of the study is rural seniors. Community care targets all vulnerable populations in need of care in the community, including the elderly, mentally ill, disabled, and homeless. However, given the aging rate and lack of care delivery systems in rural areas, this study focuses on the elderly and draws implications for the community care promotion system.
ELDERLY CARE SYSTEMS IN SOUTH KOREA
Overview of elderly care systems
The main public elderly care services in Korea are the Long-Term Care Insurance and Elderly Personalized Care Services. According to Article 1 of the Long-Term Care Act, the Long-Term Care Insurance is a social insurance system that provides long-term care benefits such as support for physical activities and household activities to the elderly who are unable to perform daily activities alone due to reasons such as old age or senile diseases, with the purpose of improving the quality of life of the elderly by promoting their health and stabilizing their lives and reducing the burden on their families. It aims to reduce the financial burden of care for the elderly in order to promote their health and stability in their later years.
The most important feature of the Long-Term Care Insurance system is its universality. It operates as a universal care system that considers the physical and cognitive functioning status of the elderly, regardless of their income, determines a rating, and provides services according to the rating. It identifies the care needs of the entire elderly population and provides services that meet the needs of each individual.
Another feature of the system is that most organizations for providing care services under the Long-Term Care Insurance are private. The National Health Insurance Service manages and operates the system, using premiums paid by the insurance subscribers and government subsidies. However, the organizations or facilities providing care are not public institutions, but private facilities established under the Elderly Welfare Act. Therefore, it is difficult to ensure sufficient supply in places where absolute demand is low and profitability is lacking, such as rural areas.
The Elderly Personalized Care Services is a care service provided by local governments that provides care for the elderly who have difficulty in performing daily activities but are not eligible for the Long-Term Care Insurance. It aims to ensure a stable old age and maintain the health and physical function of the elderly, preventing them from entering high-cost care services such as the Long-Term Care Insurance.
The Elderly Personalized Care Service is an optional care system and not all elderly people are eligible for the service. Service recipients must not be eligible for similar programs, such as those aged 65 or older who receive the National Basic Livelihood Program and the next higher tier, or those who receive the Basic Pension Program and are eligible for the Long-Term Care Insurance. For example, elderly people who need care, such as elderly people living alone, grandparents, or elderly households, or elderly people who suffer from physical decline, cognitive decline, depression, or are at high risk of loneliness or suicide, must meet certain income standards.
DEMAND FOR RURAL ELDERLY CARE
According to Table 1, it is estimated that about 1.95 million elderly people, or 24.3% of the 8.03 million elderly people aged 65 and over in Korea, are potential care seekers who have difficulty leading their daily lives. Based on the Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL), 74.7% of the elderly have no functional limitations, leaving 25.3% who need care.
Of the 1.95 million potential care seekers, we estimate that about 1.12 million are receiving public care, leaving 795,000 in the care gap. As of the end of 2019, there were 765,000 elderly people in the group receiving the Long-Term Care Insurance benefits plus 350,000 people receiving the Elderly Personalized Care Services. The total number of seniors who take the public care is about 1.12 million, or 13.8% of the total elderly and 57.2% of the elderly with potential care needs. Assuming that 30% of the elderly population aged 65 and over live in rural areas, about 240,000 elderly people do not have the chance to take the public care services.
LIMITATIONS OF RURAL ELDERLY CARE SUPPLY
The biggest problem with the care supply system in rural areas is that facilities to provide care are concentrated in cities, and rural residents' access to facilities is significantly more difficult than that in cities. As shown in Table 2, there are an average of 54.2 elderly welfare facilities per metropolitan areas, but only 19.6 in rural county areas. Social welfare facilities, including elderly welfare facilities, are also mainly located in cities, with an average of 119.9 facilities per urban cities, but only 39.6 facilities per rural town. Therefore, rural residents have to travel farther than urban seniors to access services.
Poor transportation in rural areas is also a problem. It is difficult to imagine residents with health problems traveling to care facilities by car. According to Table 3, the average number of bus trips per town per day is only 6.1, with 20 percent of the regions having fewer than three bus trips per day or no bus trips at all. The same is true for taxis, another form of public transportation. Furthermore, 78.8% of all counties have two or fewer taxis on standby. Therefore, it is virtually impossible for people living at the village level to access care facilities located in the center of a town or county in a timely manner.
COMMUNITY CARE THEORY AND PROGRAM PRACTICE
The Multidimensionality of Community Care
Community care should fulfill the following two premises. The first is that the care recipient moves from an isolated facility to the community and provides integrated care from service planning to care centered on the needs of the care recipient. The second is that the care recipient is not isolated in the community but lives as a member of the community, meaning that the care recipient participates in community activities and the community recognizes the vulnerable as a member of the community.
From this perspective, community care can be defined based on the multidimensionality of 'community' and 'care' as shown in Table 4. Community is defined in terms of three dimensions: "community as a space (in the community)," "devolution of power to localities (decentralized community)," and "community as an active subject (by the community)," and care is defined in terms of three dimensions: " medical & health care," " long-term & social care," and "social inclusion " (Kim, 2018a, 2018b).
Community as a space is deinstitutionalization. It involves moving people from institutions to the community and attempts to prevent social hospitalization, where a lack of care leads to institutionalization. It allows the community to provide care based on the person's needs, rather than forcing them to live in an institution that ignores their diverse needs.
Devolution of power to the local level means that local governments actually play an active role in planning and strategizing community care projects. It ensures that local governments have the responsibility and authority for the overall care, so that they can implement community-based care based on the needs of the recipients. Reasonable division of roles between the central government and local governments, with local governments taking responsibility for providing community-based care in partnership with the private sector.
Communities as actors is based on communities and residents taking the lead in planning and providing care, rather than having care provided by the central government or local governments. In conventional care, the government provides one-size-fits-all care and the person receiving care is not involved in the planning or delivery of care. However, community-driven care provides opportunities for not only care providers but also care recipients to participate in care to restore and revitalize their communities.
Care includes three dimensions: health care, nursing and care services, and social inclusion. Health and medical services are services such as medical treatment, nursing care, and rehabilitation provided by medical institutions under the National Health Insurance System to care recipients. Nursing and care services refer to integrated services such as housekeeping, care, nursing, and rehabilitation provided by facilities for the elderly or people with disabilities and focus on providing a variety of daily living support services. Social inclusion means supporting people in care to become part of the community by participating in jobs, leisure and sports activities, community activities, etc. in addition to direct health and medical services and nursing and care services.
CURRENT STATUS OF COMMUNITY CARE PILOT PROJECT
The pilot project was conducted nationwide in two rounds with local governments. A total of eight local governments were selected for the first round, including four models of integrated community care for the elderly, two models of independent living and community settlement for the disabled, and one model of community settlement support for the mentally ill. For the second round, two metropolitan areas, one rapidly aging area, three urban-rural complexes, and two rural areas were selected to cover a wide range of localities according to local characteristics.
The pilot project seems to focus on "deinstitutionalization" to realize community as a space. It sends care recipients currently in facilities to the community and supports them to settle and live in the community. To help those who have been discharged live in the community, residential support infrastructure is expanded, and home healthcare and home care services are provided. For example, projects targeting the elderly provide integrated medical care, and needs assessments to elderly people who have been admitted to a nursing hospital or nursing home to help them return to the community. It is aimed at elderly people who are preparing to be discharged from nursing facilities and elderly people who live in the community but are unable to enter a facility due to difficulties in their daily lives. Local governments will conduct a needs assessment and develop an individualized support plan, including a discharge plan. The hospital's local coordination office will develop a discharge plan and connect with care information centers. Home repair, home medical care, and in-home services will be provided to help the elderly with limited mobility live comfortably at home. It also emphasizes the establishment of community health centers to provide health care and comprehensive rehabilitation centers to expand long-term care at home.
Another feature of the pilot project is that it emphasizes the devolution of power to local governments, allowing them to plan and operate necessary services with autonomy. For example, city and district community care councils are responsible for selecting community care recipients, coordinating and discussing individual cases, and finalizing and implementing integrated care plans, while city, county, and district convergence service teams support the operation of community care councils. Town, village, and district care information centers provide comprehensive counseling, reception, application, and follow-up checks and inspections. Local governments at the county level have been given the authority to carry out care-related planning and financial execution, allowing local governments to carry out projects that were previously planned and operated by the central government.
However, there are limitations to implementing the project in rural areas. First of all, policies that focus on deinstitutionalization in rural areas are not effective. This is because the probability that a person discharged from a facility will settle in a rural area is extremely small. For example, if a person is admitted to a nursing home in a county, their original residence is likely to be in an urban area. the probability of returning to the rural area after discharge is extremely low because they want to live their original residence, but not rural area where they temporarily resided. This is why services targeting institutionalized persons in rural municipalities are unlikely to be effective.
There is also a problem with the emphasis on building and improving care facilities rather than the original purpose of providing welfare benefits that meet individual needs. Installing facilities in rural areas where care is scarce is positive. However, it is difficult to establish such facilities in villages with low population density, where there is neither economic benefit nor absolute demand to ensure minimum efficiency. It is clear that most of the new facilities will be located in municipal centers, and the beneficiaries of facility improvement projects are likely to be centrally located facilities. Therefore, it is difficult to establish new care facilities in rural areas, and it is difficult to attempt to improve existing facilities.
The role of local communities as drivers was also overlooked. Some of the local governments selected for the first round of pilot projects proposed using village communities or social economy organizations to provide integrated care or to match volunteers with clients. However, not only is it unclear how these plans will be implemented, but rural areas are also vulnerable to hiring people to work in social and economic organizations or finding volunteers. While this can be considered as a short-term solution, it is unlikely to be sustainable in the future without an organized workforce and decent wages.
The care recipients were also thoroughly neglected. In community-based care, trust and cooperation between caregivers and care recipients are important. However, none of the pilot municipalities had planned any organizations or projects that directly involved the recipients. Unlike cities, rural areas are characterized by local community traditions. A community care model that pursues the community as a space and the community as a subject can be completed if it is led by the local community, where care providers and care recipients coexist in accordance with the traditions of the local community. The top-down project promotion led by local governments has also excluded the role of the community as a care provider.
POLICY DIRECTION OF RURAL COMMUNITY CARE
Overview
To overcome the limitations of rural areas in the elderly care system, rural community care should be primarily community-driven. The community should be at the center of the role in providing care and overcoming the limitations of rural resources and access to resources. Conflicts between providers and recipients should be mediated within the community, and local people should be empowered to plan and organize the services they need and how they are delivered. We need to move away from the role of providing care within the public care system to one that is inclusive of all people in the community and restores a sense of community in rural areas. In rural areas where there is a history of cooperation and solidarity among local communities, community-led care can be an alternative way of addressing the challenges of rural care systems.
Based on the perspective that the community becomes the subject of care, we will discuss the direction of promoting rural community care. We would like to suggest the direction that rural community care should pursue in terms of targets, promoters, how to discover cases, how to provide care and set up facilities, and how to link with other projects.
Eligibility
The physical and cognitive functioning status of the elderly can be categorized into four main categories based on the classification of the Long-Term Care Insurance and the classification criteria for the home health care project. 'Healthy seniors' are seniors who are able to perform daily activities and have no mental or psychological problems, 'potentially ill seniors' are seniors who do not have major problems with daily activities but are experiencing some discomfort and are likely to experience a decline in physical function or cognitive status in the future, 'lightly ill seniors' are seniors who have begun to experience a decline in functional status and require simple care, and 'severely ill seniors' are seniors who are unable to perform daily activities and require full care.
The Long-Term Care Insurance provides care for seniors in critical condition. Elderly people with severe conditions are in tier 1 or 2 of the insurance and can be admitted to a nursing home or nursing hospital. Lightly ill elderly people are cared for in a home-based elderly welfare facility with levels 3-5 of the Long-Term Care Insurance. As mentioned earlier, about 765,000 elderly people receive benefits and can be cared for in long-term care facilities in rural areas.
The Long-Term Care Services are available in rural areas, but rural seniors do not have sufficient access to long-term care services, especially day care. According to elderly care experts and activists, every community with a population of 2,000 or more, or an elderly population of 700 or more, must have at least one day care center. Day care centers provide a variety of physical and social programs for those eligible for the Long-Term Care Insurance and help seniors maintain social connections. However, 67.8% of all counties in Korea and 61.9% of counties with 700 or more elderly people do not have day care centers under the Elderly Welfare Act or the Long-Term Care Act.
About 735,000 elderly people with mild conditions are eligible for personalized care services, but they are unable to receive care. In particular, about 30% of those eligible for the service live in towns and villages, so it is likely that at least 200,000 people are potentially eligible for the service but do not receive proper care. Moreover, the government has budgeted US$288.1 million for the elderly personalized care service, which is only about KRW100 million per town and village and about KRW200,000 per potential recipient. This is not enough to provide sufficient services in rural areas.
Rural community care is intended for rural elderly adults who are underserved due to a lack of long-term care and aging-in-place services, and for rural seniors who are currently healthy but are likely to decline in physical function or cognitive status in the future. Rural community care complements the aged care delivery system in rural areas and provides preventive care to prevent potential eligible from developing mild or severe conditions.
Drivers
The community care currently being discussed lacks a channel to realize the community as a subject. The Ministry of Health and Welfare's community care pilot project is led by local governments, but the problem is that local governments are not communities. In the pilot project, the local government's care center or service team is responsible for establishing the community care system and planning and coordinating the project. It is appropriate for local governments to discover and verify pioneering project models and create localized models in terms of decentralizing care. However, it is difficult for community care led by municipalities to reach rural areas at the village level, which are spatially distant.
Rural community care should be driven by residents. Local care needs are best understood by the people who have lived in the area for the longest time and by the people who are the recipients. For example, suppose there is an elderly person in your village who is not eligible for the Long-Term Care Insurance or personalized care services for the elderly, but would like a bath or lunch delivery service. If the elderly person does not actively express their needs, it is difficult to provide the service. It is difficult for municipalities and community centers that are spatially distant from the village to actively seek out and serve this person. Residents who live and interact with their neighbors are best suited to identify and connect them to public care.
To implement resident-led community care projects, you need a local community organization. Typically, these organizations include only a few recognizable residents, such as the head of the village or the village treasurer, but it is important for residents of all backgrounds to participate in community care projects. This is because the community is only sustainable if everyone agrees on the purpose and direction of the community. However, it is rare for a voluntary organization to form spontaneously in a short period of time. In fact, the Ministry of Health and Welfare's community care pilot project has a two-year duration, and after one year, care facilities have been created, but none of them are led by resident organizations. Therefore, we need to think about how to organize communities to ensure residents' participation and enable efficient community care projects.
Discovering care cases
One of the keys to community care is to identify the needs of the recipients and provide care based on their needs. In order to identify the needs of the recipients, it is necessary to discover recipients with care needs, and in the integrated care pioneering project, the care information desks of town, village, and community centers play a role. Among the cases discovered by the care information centers, those that can be managed within the town and village are solved by themselves, and those that are difficult to solve are provided with care in conjunction with the local care council of the city and district.
The problem is that it is difficult for town and village care information centers to discover cases and potential beneficiaries. The pilot project places one or two community care counselors at the community center. However, it is difficult for one or two counselors to find people who live in large areas such as towns and villages. They cannot help providing services unless the person comes to the care information center.
Rural community care puts residents in the role of connecting people with care services. Residents know their area and neighbors best and have no problem accessing clients. Local people can identify people in need and connect them with local government outreach workers or case managers. Connecting with local neighborhood councils, such as Community Security Councils, whose purpose is to identify welfare blind spots in the community can make case finding more efficient.
Provision of care
Providing care to eligible people at the village level requires setting up a care facility within the village or setting up a facility in a district center and providing transportation. Private for-profit care facilities are difficult to establish in rural areas because the absolute demand is not high enough to make it profitable. In rural villages, there are also senior centers, which are leisure welfare facilities for the elderly. However, it is difficult to call it a care facility as it only requires a space of 20 m2 or more that can be used by more than 20 people (10 people in towns and villages).
Rural community care is a system in which residents plan and provide care directly or indirectly. To provide the Long-Term Care Insurance services for the elderly or customized care services for the elderly, caregivers and support workers are needed. Villages and districts can provide care themselves if they have residents who can perform the duties of a caregiver or support worker. You can also support training courses to help them become qualified. The care needed for potentially elderly people is day-to-day care that doesn't require specialized knowledge. This type of care, such as checking in on neighbors or identifying and connecting with neighbors in need, has a long history in rural communities. More specialized care can be provided by residents who have received some education or training or are caregivers.
Rural community care focuses on the relational nature of care. Care is based on the mutual recognition of caregivers and recipients, and the quality of care is enhanced when providers and recipients work together based on trust and cooperation (Kim 2015). Care is a co-production in the sense that the quality of care is determined by the relationship between the care provider and the care recipient. From the perspective of co-production, professionals should not assess the needs of users and develop services, but users should participate as active agents who express their own needs and lead the development of services. The effectiveness of care is also higher when care is provided by a resident who understands their current condition than by someone who does not know them at all. When care is planned and delivered by people who are not currently eligible but may become eligible in the future, it is more likely to be the most appropriate and necessary care for them.
Residents who participate in care should be paid a fair price for their labor. Rural residents are primarily engaged in agriculture and cannot stop farming to provide care. If you don't compensate them for the opportunity cost of providing care, the care they provide will not be sustainable. Therefore, if they spend part of their farming time providing care, you should compensate them or hire them for part-time work or a second job.
Medical personnel, such as nurses, are needed to promote the health of the target population and manage chronic diseases. In rural areas, one organization that can play this role is a health center. Health clinics are the smallest level of public healthcare, staffed by public health officials who are nurses and hold a nursing license, according to the Special Measures for Healthcare in Rural Areas Act. There are 1,904 clinics nationwide, with each clinic covering 5-10 villages, providing good access to the target population. Medical consumer life cooperatives (hereinafter referred to as medical cooperatives) that operate in rural areas are also an alternative. However, there are difficulties with the establishment standards that do not match the reality of underdeveloped rural areas, and the system needs to be improved.
Establishment of care facilities
Rural community care projects require two types of facilities: central care facilities that provide specialized care, such as day care centers, and small village care facilities that provide the physical and emotional support needed to lead a normal life, such as assisted living, daily care, and emotional care.
It is unlikely that care facilities will be paid for by the community. A viable alternative is to utilize central government or local government community development programs, especially the Ministry of Agriculture's General Rural Development Program. The purpose of the program is to restore rural livelihoods and strengthen connections between centers by expanding investments in poor rural infrastructure. This is consistent with the goal of rural community care, which is to restore local welfare communities by expanding care infrastructure in rural areas. Under this project, facilities such as day care centers can be established in rural centers through the various project conducted in rural areas.
A day care center can be established in the center of the rural town. As mentioned earlier, there must be at least one day care center in every county that provides long-term care services. Despite this urgency, about 60-70% of all rural towns in South Korea do not have day care centers. By utilizing the development project mentioned above, a day care center can be established in the center of the county to provide high access to day care for the elderly.
Along with day care centers, care centers will be established to support rural community care. The care support center will be home to the secretariat that plans and manages community care, performing tasks such as planning care provision, operating day care facilities and village care facilities, linking with local care organizations, and researching and utilizing local physical and human resources. Providing the secretariat with a location for its activities ensures that rural community care projects are carried out efficiently.
Small-scale care facilities can be set up by improving the existing senior centers at the village level. As of the end of 2018, there were about 66,286 senior centers nationwide, many in rural areas, and they play an important role in the welfare service delivery system. However, due to their small facilities and lack of specialized staff, they only play a role in building relationships and communication within the community. Improving the facilities of these rural senior centers can help reduce the cost of building care facilities and ensure accessibility to the target population.
Transportation to care facilities can also be provided. To visit the day care center in the center of the village, transportation is needed, and the problem of transportation can be solved by using the center revitalization project, the basic living base project, and the rural transportation model visit project. Introduce a "village care bus" so that villagers can visit day care centers in the center of the county.
Linking projects
For a rural community care project to be successful, community participation is essential. If the administration plans and operates from the top down, projects that ignore the actual needs of local residents will be created, and the sustainability of the project will be lost, resulting in idle facilities and operating costs. Therefore, it is necessary to identify local resources and make plans to link various projects through direct participation of residents.
The project of establishing and implementing a resident-led village welfare plan can be used in the rural community care planning stage. Village welfare planning is a project in which towns and villages develop and implement plans for small-scale agendas that can be solved on their own, such as neighbor care and community welfare schools. Engage residents and provide educational programs so that they can actually participate.
If you have a neighborhood association, you can also utilize the neighborhood plan. In the community self-governance plan, residents participate to organize subcommittees, discover village agendas, and establish self-governance plans for each subcommittee. The welfare division can plan rural community care projects and establish mid- to long-term action plans for public discussion.
At the implementation level, it can be linked to social farming. Social farming is defined as "agricultural practices that bring the socially excluded into society" (Kim 2017), meaning agricultural activities that provide care, education, and employment to vulnerable rural populations, such as those without jobs, those with mental and physical disabilities, and those who want to learn agriculture, for the purpose of rehabilitation and self-reliance. Rural community care targets include the elderly and the chronically mentally disabled who are not cared for by the public care system. Therefore, social farming can be recognized, connected, and provided as a form of care.
The reason why social farming is effective as care is that agricultural activities are the most familiar activities in rural areas. The target audience are the rural residents. They have a lot of experiences with agricultural activities and social interactions, so they can easily adapt. Social farms are also easy to access because they are located in rural areas. Instead of having to travel to the center of town for occupational therapy, they can participate in social farming programs offered by their neighbors. In fact, the social farms selected for the 2020 Social Farming Revitalization Support Project provide social farming programs for the underprivileged in rural areas, such as people with dementia, people living alone, people with disabilities, farmers and villagers, and young farmers. Collaborating with neighboring social farms provides an opportunity to improve the effectiveness of community care.
CONCLUSION AND FUTURE CHALLENGES
The key to rural community care is that it is driven by local communities, not institutions. It centers on the community and provides care to those who do not receive sufficient care in the existing care delivery system, or who need preventive care but do not receive public care benefits. Plan care from the perspective of the care recipient and provide care to their neighbors. Coordinate with other community organizations and local governments to provide efficient care. It is the role of the caring community to strive to provide diverse and effective care by installing and operating care facilities and providing social farming programs in conjunction with agricultural businesses.
Support caring communities to create a secretariat to run rural community care. A top-down system of care is possible when caring communities are supported to create a secretariat to run community care. Because caring communities are organized by residents, they need to organize and set up a secretariat with expertise. The secretariat can perform a variety of tasks, including conducting needs assessments, running and evaluating facilities, and engaging and collaborating with the community. These tasks need to be carried out with professionalism and continuity, which requires a full-time person in the secretariat and adequate compensation for the full-time person. Therefore, the caring community should be supported by the central government or local government in hiring and running the secretariat staff.
Rural community care is a bottom-up system of care. Rather than central government or local governments planning and delivering care, it is a system that supports communities of people to plan and run their own care. In the early stages of the project, community learning organizations and the communities they organize will be supported in a phased manner. Support the learning organization to identify care needs in the village and create a care plan that considers the local context. Then, once the learning organization is transformed into a community care organization, we provide subsidies to help them set up and operate care facilities and pay for care workers. Only by operating from the bottom up can community care become a sustainable rural care delivery system.
From this point of view, a social economic organization, in particular a social cooperative, may be the most appropriate legal entity for the community. When a community becomes a social cooperative, care recipients and providers can operate in the same community in cooperation and solidarity for the purpose of providing care based on co-production (Cho 2014), and both recipients and providers can participate in the management of the community as subjects, ensuring the sustainability of the community. Therefore, social cooperatives can be an alternative way to lead rural community care.
In conclusion, rural community care is defined as "a system in which a caring community, a resident care organization, with the participation of all residents, utilizes existing human and physical resources and subsidized projects provided by the government to provide preventive care to the recipients and include the recipients in the community". It is a system in which resident community organizations plan projects with the central government and local governments and use a combination of internal and external physical and human resources to provide professional care, daily support, health promotion programs, and chronic disease management.
Future research challenges include First, the actual needs of rural elderly people should be investigated and services should be planned. It is necessary to investigate the actual care needs of rural elderly people and plan service provision accordingly, such as entering facilities such as nursing homes, expanding the Long-Term Care Insurance and elderly-specific care services, establishing day care centers, providing home-based care and daily care, expanding health-related programs per elderly person, and increasing community activities.
Caring communities should be provided with specific information about what they need to do to implement rural community care. If there are local residents who are interested in rural community care, they should be provided with accurate information in order to provide services. In particular, specialized information such as how to set up and operate a care facility and the care delivery system should be provided. For example, you should provide specific information on the actual cost of the care facility, the hiring of staff, the legal status of the operating entity, and the utilization of subsidized projects. Only when communities have this information can they plan and operate their care provision, reducing the risk of failure and increasing the likelihood of success.
Finally, rural communities need to be mindful of central government programs and ensure that they can continue even if funding is cut off. Care in rural areas is particularly difficult to monetize, making it unlikely that private organizations or facilities will be able to enter the market. Therefore, care support projects implemented by the Ministry of Health and Welfare or local governments should be coordinated. For example, rural community care can be provided with support from the Ministry of Health and Welfare or local governments, including care for the severely ill. Sustainability issues should be considered not only by the Ministry of Health and Welfare, but also by the Ministry of Agriculture.
REFERENCES
Cho, M. (2014). Feasibility Exploration of Social Cooperatives as a Community Social Work Practice Model. Journal of Agricultural Extension & Community Development, 21(3), 91-119.
Health Insurance Review and Assessment Service. (2019). Health Insurance Statistical Year Book.
Jung, K., Oh, Y., Lee, Y., Oh, M., Kang, E., Kim, K., Hwang, N., Kim, S., Lee S., Lee, S., & Hong, S. (2017) Survey on the Elderly. Korea Institute for Health and Social Affairs.
Kim, E. (2015). A community approach for establishing the effective social care system. Korean Journal of Social Welfare Studies, 46(2), 153-176.
Kim, J., An, S., Lee, J., & Kim, K. (2017). Social Farming in Rural Korea and Policy Direction. Korea Rural Economic Institute. 1-121.
Kim, Y. (2018a). Deinstitutionalization and Building Community-Based Personal Social Services: Community Care that Connects Independence and Interdependence. Health and Social Welfare Review, 38(3), 492-520.
Kim, Y. (2018b). Community care, what to do and how to do it? Welfare Trend, 238, 5-10.
Ministry of Health and Welfare. (2019a). 2019 Status of Welfare Facilities for the Elderly
Ministry of Health and Welfare. (2019b). Community Integrated Care (Community Care) Pilot Project initiative.
National Health Insurance Service. (2018). Long Term Care Insurance Statistical Year Book.
National Health Insurance Service. (2019). Average length of stay in nursing homes and assisted living facilities by state for persons aged 65 and older in 2018.
Statistics Korea. (2020). 2020 Census of Agriculture, Forestry and Fisheries.
Statistics Korea. (2019a). 2018 Population and Housing Census.
Statistics Korea. (2019b). Statistics for seniors.