ABSTRACT
The promotion of healthier dietary patterns has currently become an important concern for Thai public health. This article is a review of the current transition in dietary patterns and nutrition status in Thailand together with food consumption trends of Thai consumers. It is found that the transition has led Thais to diet-related chronic diseases particularly obesity and overnutrition resulting in massive health care costs. Although the consumption in Thailand has been involved with more eating in ready-to-cook/eat foods, food away from home and unhealthy foods which is attributable to the change in socio-economic patterns such as increase in smaller size households, increase in female labor force and a higher role of modern retail, some Thai consumers are becoming more aware of healthy lifestyles and begin to demand for healthy foods. The challenge for the Thai government is to provide policy measures to improve healthier diets for their population and reduce the socio-economic inequity in access to healthy foods.
Keywords: Dietary patterns, Food Consumption Trends, Consumer Policies, Healthier Diets
INTRODUCTION
Thailand is a Southeast Asian country which has experienced a socio-demographic and economic transformation over the last few decades. The said transformation is a consequence of trade liberalization and globalization. This change has influenced the lifestyles of the Thai population particularly their dietary patterns and nutrition status. Since the 1990s, food consumption of Thai consumers has shifted from traditional Asian foods with high fiber and low fat content towards Western diets with high proportion of meats, fats and sugar(Aekplakorn, 2010; Kosulwat, 2002).
The noticeable shift in calorie intake of Thai population has been observed because calories from staple food share have been replaced by energy consumption from protein and fat. At the same period, the Thai people have moved from eating whole grain cereals and fiber, especially rice, to more refined carbohydrates such as sugar. The sugar intake of Thais has become an interesting issue owing to the information that the amount of intake has increased nearly threefold within only 30 years and the present consumption has been found to begin excess of the recommended level by the Thai Recommended Daily Intakes (Thai RDI) by four times (Food and Agriculture Organization, 2017).
Along with the changes in dietary pattern of the Thai population, Thailand has reached an important point in nutritional and health transition. Overnutrition, together with a reduction in physical activities, especially in activities associated with occupation and commuting among the population, has driven the prevalence of being overweight and obesity in Thailand. A report from the National Health Examination Survey showed that the percent of overweight and obese Thai adults with age 15 years and over increased dramatically from 20.4% in 1991 to nearly 50% in 2009 (Aekplakorn et al., 2014). This occurrence has not only happened in adults but has also grown continuously among Thai children. In 2009, the proportion of being overweight obesity in pre-school children and primary-school children aged between 6 and 14 years were 8.5% and 9.7% respectively (Chavasit, Kasemsup, & Tontisirin, 2013).
Aside from obesity, overnutrition has resulted in many diet-related chronic diseases such as diabetes, cardiovascular disease, hypertension, stroke and cancer (World Health Organization 2006) It is one of the main contributors to the burden of chronic diseases and disability of Thais and reduces the overall quality of Thai population’s life.The rapid emergence of obesity and other diet-related diseases have become increasingly important public health priorities (Aekplakorn et al., 2007; Wilbulpolprasert, 2008).This occurrence can lead to large health care costs both in developed nations and developing countries. The WHO has estimated that overnutrition accounted for 2-6% of total health care costs in several countries. The total cost attributable to obesity in Thailand was estimated at proximately 12,142 million baht which accounted for 0.13% of Thailand’s Gross Domestic Product (GDP)(Pitayatienanan et al., 2014).
The nutrition transition in Thailand has become an important concern for better health. Nowadays, energy dense, processed and Westernized foods are widely available and affordable throughout the country to all socio-economic consumer groups through the agency of transnational food company investments. However, higher income and more educated consumers are beginning to demand for more diverse and healthier diets just like the situation in more developed countries. The challenges for the Thai government and public health officials are to provide effective nutrition education and to boost affordable healthy diets for their population together with avoidance of the socio-economic inequity of nutritional outcome as observed in many rich nations(Kelly et al., 2010).
TRANSITION IN DIETARY PATTERNS AND NUTRITION STATUS
Similar to other countries in the Asia and Pacific region, Thailand has encountered socio-demographic and economic transitions. During this era, industry and services have replaced agriculture as the main sector of Thai economy. The social structure of Thais has also changed from a rural orientation to an urbanized society which creates changes in family and population ageing structures. The upward trend of small families has been observed and the population has changed from a mainly young population to an increased proportion of adults and the elderly (Kosulwat, 2002).
Rapid socio-economic transition together with the introduction of urbanization and Westernization has also influenced the lifestyles of the Thai population, particularly their dietary patterns. Previously, traditional Thai cuisine mainly consisted of rice and fish; while other types of meat were rarely included in any dishes. Basic ingredients such as fresh spices and herbs were commonly added to most Thai dishes. For a typical Thai meal, there are no “courses” instead; the dishes are served at the same time to complement each other. All side dishes are eaten with rice, which is the Thai main staple. During the transition period, eating patterns in Thailand have shifted from traditional Asian food with high cereal and low fat content towards Western diets consisting of a high proportion of meat, fats and sugar as similarity to transition in many Asian countries (B.M. Popkin, 2002; Barry M Popkin, 2004).
The transition of food consumption pattern in Thailand is demonstrated in Table 1. This table indicates the growth of meat, fish, dairy products and sugar consumption between 1975 and 2010. As a consequence of more animal product consumption, fat intake of Thais from animal sources has nearly doubled. Thai population has consumed dairy products including milk increasingly from only 19 grams/day in 1975 to 72 grams/day in 2010; whereas, the overall consumption of cereal and rice declined. People have moved from eating whole grain cereals and fiber, especially rice, to more refined carbohydrates such as sugar. Sugar intake emerges as an interesting issue for the current situation because the amount of intake has increased nearly threefold within only 30 years. In 2010, the daily sugar intake of Thais was up to 107.67 grams that was in excess of the recommended Thai RDI level (24 grams per day for added sugars) by nearly five times.
Table 1. Changes in food consumption in Thailand from 1975 to 2010
Unit: quantity/day/capita (g)
|
|
Year
|
|
|
Food item
|
1975
|
1985
|
1995
|
2005
|
2010
|
|
Rice & cereals
|
439.18
|
348.22
|
337.81
|
388.77
|
374.25
|
|
Rice
|
435.07
|
322.19
|
304.38
|
322.19
|
315.34
|
|
Vegetables
|
146.85
|
113.42
|
122.19
|
133.70
|
135.89
|
|
Fruits
|
246.58
|
258.63
|
255.62
|
318.63
|
292.33
|
|
Sugar & sweeteners
|
33.97
|
38.63
|
74.79
|
88.22
|
107.67
|
|
Meats
|
47.67
|
58.90
|
76.71
|
76.16
|
76.99
|
|
Fish & seafood
|
55.07
|
55.07
|
85.48
|
91.78
|
65.48
|
|
Milk
|
18.90
|
25.21
|
70.68
|
70.14
|
72.05
|
|
Fat from animal source
|
12.03
|
16.12
|
21.44
|
21.61
|
24.72
|
|
Fat from plant source
|
3.56
|
8.49
|
15.07
|
17.81
|
20.82
|
Source: Food and Agriculture Organization (2017)
It is not surprising that the energy consumption patterns of the Thai population have also changed during the transition period. Table 2 demonstrated the change in calorie and macronutrient intakes of Thai consumers from 1970 to 2010. The overall daily energy intake of Thais increased by approximately 590 kcal between 1980 and 2010 although it dropped down a little bit previously. An examination of macronutrient composition indicates that energy consumption from staple foods (carbohydrates) was replaced by calories from protein and fats. Thai consumers had the share of energy from protein around 9% of total energy. At the same time, the share of energy from fat in Thailand was nearly doubled and was supposed to grow continuously.
Table 2. Trends in dietary intake of energy, protein, fat and carbohydrate in Thailand from 1975 to 2010
Unit: kcal/day/capita
|
|
Year
|
|
|
1970
|
1980
|
1990
|
2000
|
2010
|
|
Energy (kcal)
|
2190
|
2170
|
2180
|
2604
|
2756
|
|
Protein (kcal)
|
205.72
|
193.52
|
196.92
|
237.76
|
236.40
|
|
As percentage of energy
|
9.39
|
8.92
|
9.03
|
9.13
|
8.58
|
|
Fat (kcal)
|
262.17
|
283.41
|
409.95
|
493.11
|
534.87
|
|
As percentage of energy
|
11.97
|
13.06
|
18.81
|
18.94
|
19.41
|
|
Carbohydrate (kcal)
|
1722.11
|
1693.07
|
1573.13
|
1873.13
|
1984.73
|
|
As percentage of energy
|
78.64
|
78.02
|
72.16
|
71.93
|
72.01
|
Source: (Food and Agriculture Organization (2017))
Most developing countries have undergone major socio-economic transition in the past three decades and now, they are approaching the post-transitional era. One worrying trend that has emerged during the transition is the “double burden” of malnutrition. Wherein undernutrition in some parts of the population co-exists with overnutrition and obesity in other segments(B.M. Popkin, Paeratakul, & Ge, 1995). Before the era of transition, the developing world had a high prevalence of undernutrition but socio-economic development together with the influences of urbanization and Westernization have shifted both the dietary and activity patterns of population, creating an upward trend in the incidence of obesity. Interestingly, this “double burden” exists not only at the country level but also at the household level(Kapoor & Anand, 2002).
The double burden of malnutrition during the nutrition transition has likely been related to the transition of epidemiology because overnutrition leads people to encounter non-communicable and degenerative diseases, while undernutrition has been associated with communicable diseases and reduction of productivity. The WHO noted that overnutrition and obesity are the major contributors to diet-related chronic diseases such as diabetes, cardiovascular disease, hypertension, stroke and cancer(World Health Organization 2006). Nowadays, stroke, heart disease and diabetes are among the top causes of mortality in Thailand (Porapakkham et al., 2010). Dietary risks are indicated as the important key factor of Disability-Adjusted Life Years (DAILs) lost for Thai population.
The trend of becoming overweight and obesity of Thai adults between 1991 and 2009 is shown in Fig. 1. This figure demonstrates that the prevalence of being overweight and obesity among Thai adults aged 15 years and over increased dramatically. The number of Thai adults who was overweight or had BMI ≥ 25 kg/m2has increased by 17.5% in 2009 compared to 1991. In 2009, the rate of obese adults having BMI ≥ 30 g/m2was 9.1%. It means that nearly 1 in 10 adults in Thailand have a tendency to face the obesity epidemic. As classified by gender, Thai females had a higher rate of being overweight and obese than males did over the period but the growth rate of this prevalence in males was up to 2.5 times while in females was double. In 2009, nearly half of Thai female adults tended to have their BMI larger than 25 g/m2 (Fig. 2)
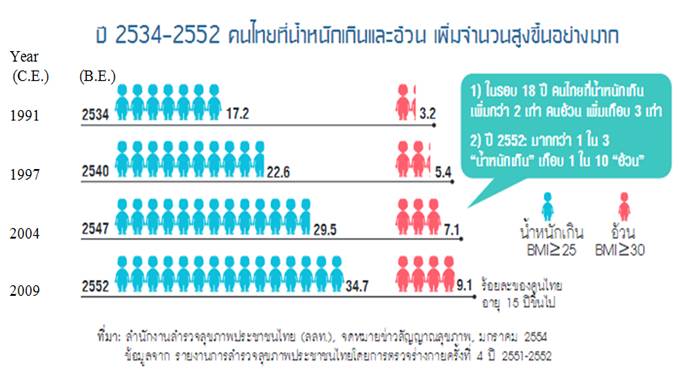
Fig. 1. The prevalence of overweight and obesity of Thai adults between 1991 and 2009
Source:ThaiHealth (2014)
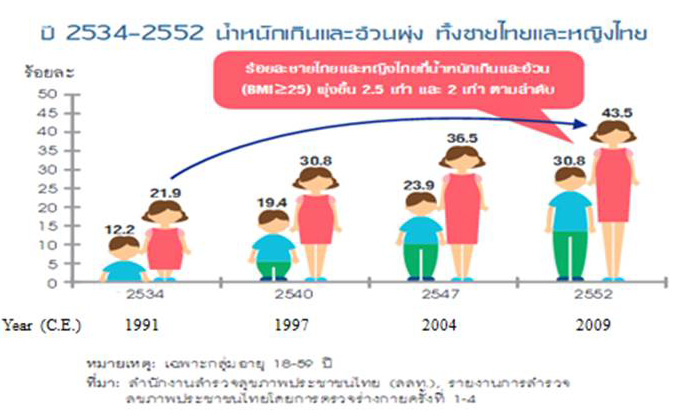
Fig. 2. The percentages of male and female Thai adults with BMI ≥ 25 kg/m2from 1991 to 2009
Source:ThaiHealth (2014)
FOOD CONSUMPTION TRENDS IN THAILAND
The linkage between food consumption and nutritional status of consumers is complex. Increased food consumption does not necessarily translate into better health and nutritional status. One of the important indicators of food security at either national or household levels is household food expenditure. A lower share of food expenditure in total spending can indicate better food security of households; however, the patterns of food expenditure in different food categories are needed to gain insights into changes in nutrition. The common factors affecting household or individual food consumption are: food prices; household income; food habits; cultural food beliefs; nutritional knowledge; food industry marketing and advertisements; tastes and preferences.
In Thailand, changes in socio-demographic patterns such as the increase in smaller sized households, increase in the female labor force, Westernization and urbanization have shifted consumers from having Thai staples with side dishes to consumption of foods with higher fats, animal meats, and less vegetables and fruits. The possible reason is that traditional Thai food requires lots of preparation time and many ingredients for cooking. Currently, Thai people tend to select food that needs less time and skill to prepare, so homemade meals, which were commonly seen in the past, have been replaced by ready-to-cook/eat foods and food away from home.
Food expenditure pattern of Thai households is showed in Table 3.This table indicates that average household size in Thailand became smaller during the period 1990 to 2010.Although the main share of food expenditure came from food at home, the share on this category decreased dramatically. At the same time, the overall expenditure on ready-to-eat food and food away from home rose over the period. The share on these two categories together increased from 24% to 46% within 24 years. An interesting point is the shaped growth of the share on ready to eat food of Thai households. Although the share on this category was only 8.8% of total food expenditure in 1990, Thai households tended to spend more on this category over the period. In 2014, the expenditure on this food group accounted about 21% of total food expenditure as well as it had a tendency to be nearby the share on food away from home category. In line with global market, convenient and ready to eat processed food products will become increasingly popular in Thailand due to lifestyle changes.
Table 3. Average expenditures spent on food prepared at home, prepared food taken home and food eaten away from home between 1990 and 2014inThailand (Nominal values)
Unit: Baht /month/ household
|
Type
|
Year
|
|
|
|
|
1990
|
1994
|
1998
|
2002
|
2006
|
2010
|
2014
|
|
Food prepared at home
|
1,494
|
1,881
|
2,609
|
2,397
|
2,491
|
3,056
|
3,491
|
|
%
|
(75.95)
|
(72.82)
|
(70.88)
|
(65.37)
|
(59.24)
|
(58.53)
|
(54.46)
|
|
|
|
|
|
|
|
|
|
|
Prepared food taken home
|
173
|
251
|
397
|
506
|
611
|
917
|
1,308
|
|
%
|
(8.80)
|
(9.72)
|
(10.79)
|
(13.82)
|
(14.53)
|
(17.56)
|
(20.41)
|
|
|
|
|
|
|
|
|
|
|
Food eaten away from home
|
300
|
451
|
675
|
763
|
1,103
|
1,248
|
1,610
|
|
%
|
(15.25)
|
(17.46)
|
(18.33)
|
(20.81)
|
(26.23)
|
(23.91)
|
(25.13)
|
|
|
|
|
|
|
|
|
|
|
No. of members in households
|
4.1
|
3.8
|
3.7
|
3.5
|
3.4
|
3.3
|
3.1
|
|
|
|
|
|
|
|
|
|
Note: Numbers in parentheses are the percentages of total food expenditure.
Source: Report of household socio-economic survey, 1990-2014
Owing to the prevalence of excessive sugar consumption, public health authorities in both developed and developing countries have investigated the patterns and trends in sugar consumption in their populations. One of the issues raised is about the largest sources of sugar in diets. Interestingly, the main source of added sugar in diets is not from eating desserts or consumption of raw sugar, but from the consumption of sugar sweetened beverages. Data from the National Cancer Institute in the United States indicates that nearly half of American sugar consumption comes from sugar-sweetened beverages with 36% from carbonated and functional drinks and 11% from fruit juices. Other sources of added sugar intake such as desserts and raw sugar account for only 19% and 3% respectively of total sugar intake. As in the US, a previous research conducted in Thailand showed that 60% of sugar consumption of Thai students resulted from drinking beverages with added sugars. The amount of sugar consumed from sugar-sweetened beverages was three and four times, respectively of that consumed from bakery items and Thai sweets- the second and third most important sources of sugar in Thai diets (Fig. 3).
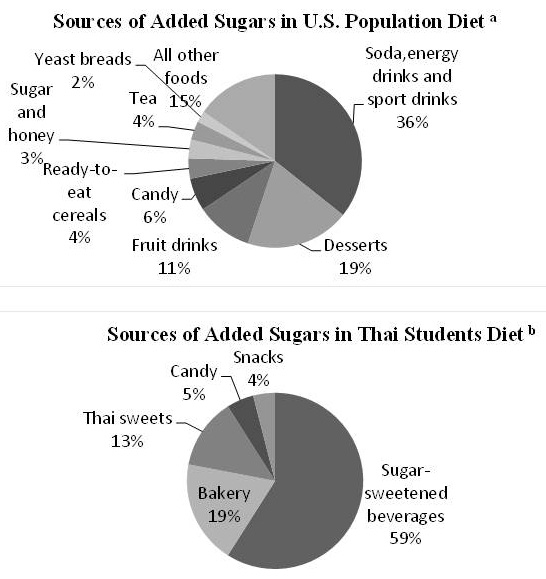
Fig. 3. Sources of added sugar diets in U.S.A. and in Thailand
Note : a Data are drawn from “Sources of added sugars in the diets of the U.S. population ages 2 years and older”, NHANES 2005–2006 conducted by National Cancer Institute (2006)
bData are drawn from “Sucrose consumption in Thai undergraduate students” by Promdee, Trakulthong, and Kangwantrakul (2007)
The change in expenditure on sugar-sweetened beverages in Thailand is also captured in this paper. Table 4 presents the expenditure on non-alcoholic beverages of Thai households, which mostly consists of beverages with added sugars. This increased by four times during 16 years and the expenditure share for this item as compared to total food expenditure increased continuously over time. Euromonitor indicates that the consumption of non-alcoholic beverages mostly composed of beverages with added sugars has also risen and is expected to grow continuously until 2014(Euromonitor International, 2010).
Table 4. Averages expenditure and shares for non-alcoholic beverages between 1998 and 2014
Unit: Baht /month/ household
|
|
year
|
|
|
1998
|
2002
|
2006
|
2010
|
2014
|
|
Monthly household expenditure for
|
78.98
|
98.50
|
236.31
|
244
|
318
|
|
non-alcoholic beverages
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Share for non-alcoholic beverages (%)
|
0.88
|
1.03
|
1.60
|
1.64
|
1.73
|
|
|
|
|
|
|
|
|
No. of members in households
|
3.7
|
3.5
|
3.4
|
3.3
|
3.1
|
|
|
|
|
|
|
|
Source: Calculated from Socio-Economic Surveys, 1998-2014
More than 80 % of Thai consumers today have access to supermarkets. The growth in access might be the result of urban movement of the population and increasing supermarket presence in non- urban areas. The association between frequent supermarket shopping and consumer group with urban residence and higher income is present in Thailand. Moreover, frequent shopping at supermarkets and convenience stores tends to be involved with the consumption of six “problem foods” (sugar-sweetened beverages, snacks, processed meats, Western style bakery products, instant foods and deep fried foods)(Kelly, Seubsman, Banwell, Dixon, & Sleigh, 2014). These foods commonly are energy dense and consist of high fat, sugar and salt that are associated with adverse impacts on health. In the same way, the WHO notes that the problem of being overweight and obesity is due to the fast change in lifestyle leading to the upward trend of eating out, eating ready to eat food cooked from local markets and food hawkers, and drinking soft drinks with high amounts of sugars. These foods are often low in nutritional value, but calorie dense and can cause overnutrition(World Health Organization, 2007).
However, the role of modern retail also has a positive impact on diets. The globalized food chains increase the diversity of food products available to consumers which induce to the potential for improvements in diet of population. The process of divergence of diets leads Thai consumers to begin a demand for more healthy foods (Kelly et al., 2010). The growing awareness of the healthy lifestyle results in an increasing demand for food items which not only provide basic nutrition but also support health. The report from THAILAND BOARD OF INVESTMENT (2013)indicates that Thai domestic market has strong demand for healthy food products. In 2011, Thai consumers spent around US$1.7 billion (or 56.5 billion baht) on health foods including sport nutrition, vitamin and dietary supplements, weight management, herbal products and allergy care foods. Even in snacks, there is an increase of health and wellness snacks. Many manufacturers have tried to reformulate their products reducing the amount of salt, sugar and fat in their products to respond the upward demand from Thai consumers for healthier snacks.
POLICY INTERVENTIONS TO PROMOTE HEALTHIER DIETS
Unhealthy dietary pattern of population can result in many diet-related chronic diseases such as diabetes, cardiovascular disease, hypertension, stroke, cancer and obesity. It can translate into a bigger burden for the government particularly in terms of large health care cost, lower quality of life and lost production. Policy interventions which are better suited can improve diets of population. Nutritional labeling which allows for informed choice is applied as one way to address the problem of unhealthy consumption in Thailand. In 2016, the Thai Ministry of public health issued a new regulation regarding food nutritional labeling to provide guidance of important nutritional information with Guideline Daily Amount (GDA)(Dachprasat, 2016). The GDA is a guideline for labeling the total amount of energy intake and some important nutrients (quantity of fat, sugar and sodium (or salt)) that may raise the risk of developing some diet-related diseases on the front of product package The GDA labeling is expected to help consumers on planning a healthy balanced consumption. It is believed that the nutritional knowledge related to consumer’s need and easy to understand is an essential factor to help consumer make an appropriate decision and help empowering them with the informed choice to have a balance diet. Example of GDA labeling on food product packages according to the notification is shown in Fig. 4.
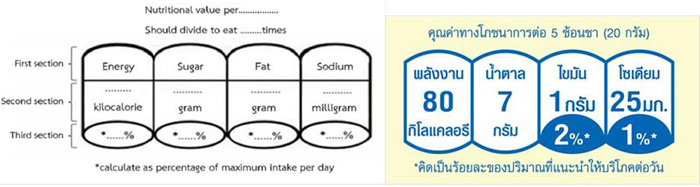
Fig. 4. Example of GDA labelling on food product packages according to the notification
Source: Thailand Publishes New Regulation For Guideline Daily Amount (GDA) Labeling by (Dachprasat (2016))
However, informed choice does not necessarily bring about consumption of healthier foods although consumers know and are able to read and interpret nutritional labeling on food purchased. Interventions targeting the market environment such as fiscal measures might be generally more effective even though it is more intrusive (Brambila-Macias et al., 2011). Recently, Thai government introduced a tax on sugar-sweetened beverages because it is believed that consumers will cut back on consuming these product items and this method can reduce the health risks such as obesity and diabetes. Under the NRSA’s proposal, the retail price of this category will be increased by 20% to 25% (Bhadrakom, 2016). However, my previous research demonstrates that the higher price might not reduce excessive drinking of sugar-sweetened beverages due to the evidence of “habit formation” driving the consumption of these products in Thailand (Bhadrakom, 2014).
According to my study (Bhadrakom, 2014), the proposed tax on sugar-sweetened beverages would lead to only modest reductions in sugar consumption around 2.12 to 2.56 g/day in the case of adults and 3.61 to 4.36 g/day in the case of children. The larger values of long-run price elasticities in relation to short-run elasticities suggest that government revenues from the proposed tax would be lower over the long run. The tax would, however, not be regressive in terms of impact on lower income categories. Therefore, changing a formulated dietary habit takes time and requires other supportive measures. Fiscal measures will need to be supplemented by nutrition education, particularly for the younger age groups, to produce a significant reduction in unhealthy food consumption.
CONCLUSION
This article has reviewed the transition in dietary patterns and nutrition status in Thailand as a result of economic development and rapid urbanization during the past decades. The transition has been associated with significant shifts in dietary intake of Thai population characterized by an increase in fats, energy dense food and excessive sugar. The socio-economic transition has led Thai consumers to encounter non-communicable and diet-related chronic diseases such as diabetes, cardiovascular disease, stroke, cancers and obesity.
Furthermore, this article has also reviewed the trend of food consumption in Thailand. We found that Thai people tend to select food which needs less time and skill to prepare. Therefore, food expenditure of Thai households on food prepared at home has been replaced by ready-to-cook/eat foods and food away from home. The excessive sugar consumption of Thais is also raised as an important issue for public health today. Previous papers report that the main source of added sugar in diet is from drinking sugar-sweetened beverages. Compared to total food expenditure, Thai households tend to spend more on this category continuously over time. Moreover, the role of modern retail gives an impact on food consumption pattern of Thai population. Frequent shopping at supermarket and convenience stores is involved with the consumption of six “problem foods” (sugar-sweetened beverages, snacks, processed meats, western style bakery products, instant foods and deep fried foods). On the other hand, the globalized food chains increase the diversity of food products available to consumers to potential for improvements in their diet. Nowadays, some parts of Thai consumers begin a demand for healthy foods and they have a growing awareness of the healthy lifestyle.
For the final point, we have talked about the policy interventions to promote healthier diets in Thailand. Recently, Thai government issued a new regulation regarding food nutritional labeling with GDA and fiscal measure as a tax on sugar-sweetened beverages. These measures are believed to reduce the consumption of unhealthy foods and cut health risks from diet-related chronic diseases. However, the measures will need to be supplemented by nutrition education particularly for the young children because food habits in early stages of life determine practices and preferences in adulthood. The consumption at schools needs to be addressed for example reduction in students’ access to sugar-sweetened beverages and unhealthy snacks. Moreover, another challenge of Thai government is to boost affordable healthy diets for their population and reduce the socio-economic inequity of nutritional outcomes due to cost constraints in poorer consumers.
REFERENCES
Aekplakorn, W. (2010). National health examination survey IV report 2008-2009. Thailand: The Graphico system co, Ltd.
Aekplakorn, W., Hogan, M. C., Chongsuvivatwong, V., Tatsanavivat, P., Chariyalertsak, S., Boonthum, A., . . . Lim, S. S. (2007). Trends in Obesity and Associations with Education and Urban or Rural Residence in Thailand. OBESITY 15(2), 3113-3121.
Aekplakorn, W., Inthawong, R., Kessomboon, P., Sangthong, R., Chariyalertsak, S., Putwatana, P., & Taneepanichskul, S. (2014). Prevalence and trends of obesity and association with socioeconomic status in Thai adults: national health examination surveys, 1991–2009. Journal of obesity, 2014.
Bhadrakom, C. (2014). Economic analysis of overnutrition in Thailand. University of Reading.
Bhadrakom, C. (2016, 15 Jun 2016). A sugar tax is not the answer to obesity Bangkok Post. Retrieved from https://www.bangkokpost.com/opinion/opinion/1010545/a-sugar-tax-is-not-t...
Brambila-Macias, J., Shankar, B., Capacci, S., Mazzocchi, M., Perez-Cueto, F. J. A., Verbeke, W., & Traill, W. B. (2011). Policy Interventions to Promote Healthy Eating: A Review of What Works, What Does Not, and What is Promising. Food and Nutrition Bulletin, 32(4), 365-375. doi: 10.1177/156482651103200408
Chavasit, V., Kasemsup, V., & Tontisirin, K. (2013). Thailand conquered under‐nutrition very successfully but has not slowed obesity. Obesity reviews, 14(S2), 96-105.
Dachprasat, N. (2016). Thailand Publishes New Regulation For Guideline Daily Amount (GDA) Labeling from www.foodsafety.sgs.com
Euromonitor International. (2010). Non-alcohol beverages in Thailand. Retrieved Aug, 11, 2012, from http://www.portal.euromonitor.com/portal/default.aspx
Food and Agriculture Organization. (2017). FAO Food Balance Sheets. Retrieved 10/6/2018, from United Nations
Kapoor, S., & Anand, K. (2002). Nutritional transition: a public health challenge in developing countries. Journal of epidemiology and community health, 56(11), 804-805.
Kelly, M., Banwell, C., Dixon, J., Seubsman, S.-a., Yiengprugsawan, V., & Sleigh, A. (2010). Nutrition transition, food retailing and health equity in Thailand. Australasian epidemiologist/Australasian Epidemiological Association, 17(3), 4.
Kelly, M., Seubsman, S.-a., Banwell, C., Dixon, J., & Sleigh, A. (2014). Thailand's food retail transition: supermarket and fresh market effects on diet quality and health. British Food Journal, 116(7), 1180-1193.
Kosulwat, V. (2002). The Nutrition and Health Transition in Thailand. Public Health Nutr., 5, 183-189.
National Cancer Institute. (2006). Sources of added sugars in the diets of the U.S. population ages 2 years and older,NHANES 2005–2006. Risk Factor Monitoring and Methods. Cancer Control and Population Sciences. . Retrieved August 11, 2012, from http://riskfactor.cancer.gov/diet/foodsources/added_sugars/table5a.html.
Pitayatienanan, P., Butchon, R., Yothasamut, J., Aekplakorn, W., Teerawattananon, Y., Suksomboon, N., & Thavorncharoensap, M. (2014). Economic costs of obesity in Thailand: a retrospective cost-of-illness study. BMC health services research, 14(1), 146.
Popkin, B. M. (2002). An overview on the nutrition transition and its health implications: the Bellagio meeting. Public health nutrition, 5(1A), 93.
Popkin, B. M. (2004). The nutrition transition and the global shift towards obesity. Diabetes in Society, 49(3).
Popkin, B. M., Paeratakul, S., & Ge, K. (1995). A review of dietary and environmental correlates of obesity with emphasis on developing countries. Obesity Research, 3, 145-153.
Porapakkham, Y., Rao, C., Pattaraarchachai, J., Polprasert, W., Vos, T., Adair, T., & Lopez, A. D. (2010). Estimated causes of death in Thailand, 2005: implications for health policy. Population Health Metrics, 8(1), 14.
Promdee, L., Trakulthong, J., & Kangwantrakul, W. (2007). Sucrose consumption in Thai undergraduate students. Asia Pac J Clin Nutr, 16(Suppl 1), 22-26.
ThaiHealth. (2014). "Self-management Communities:" Foundation of National Reform. Nakhon Pathom , Thailand: Institute for Population and Social Research , Mahidol University.
THAILAND BOARD OF INVESTMENT. (2013). Thailand’s Food Industry: THAILAND BOARD OF INVESTMENT.
Wilbulpolprasert, S. (2008). Thailand Health Profile 2005–2007. Bangkok: Ministry of Public Health.
World Health Organization (2006). Obesity and Overweight. Retrieved June 10, 2010, from http://www.who.int/mediacentre/factsheets/fs311/en/print.html
World Health Organization. (2007). Thailand National Health System Profile 2007. Retrieved March 12, 2012, from http://www.searo.who.int/LinkFiles/Thailand_Thailand_final_031005_WT.pdf
|
Date submitted: July 11, 2018
Reviewed, edited and uploaded: Sept. 10, 2018
|


Trends in Dietary Patterns and Consumer Policies in Thailand
ABSTRACT
The promotion of healthier dietary patterns has currently become an important concern for Thai public health. This article is a review of the current transition in dietary patterns and nutrition status in Thailand together with food consumption trends of Thai consumers. It is found that the transition has led Thais to diet-related chronic diseases particularly obesity and overnutrition resulting in massive health care costs. Although the consumption in Thailand has been involved with more eating in ready-to-cook/eat foods, food away from home and unhealthy foods which is attributable to the change in socio-economic patterns such as increase in smaller size households, increase in female labor force and a higher role of modern retail, some Thai consumers are becoming more aware of healthy lifestyles and begin to demand for healthy foods. The challenge for the Thai government is to provide policy measures to improve healthier diets for their population and reduce the socio-economic inequity in access to healthy foods.
Keywords: Dietary patterns, Food Consumption Trends, Consumer Policies, Healthier Diets
INTRODUCTION
Thailand is a Southeast Asian country which has experienced a socio-demographic and economic transformation over the last few decades. The said transformation is a consequence of trade liberalization and globalization. This change has influenced the lifestyles of the Thai population particularly their dietary patterns and nutrition status. Since the 1990s, food consumption of Thai consumers has shifted from traditional Asian foods with high fiber and low fat content towards Western diets with high proportion of meats, fats and sugar(Aekplakorn, 2010; Kosulwat, 2002).
The noticeable shift in calorie intake of Thai population has been observed because calories from staple food share have been replaced by energy consumption from protein and fat. At the same period, the Thai people have moved from eating whole grain cereals and fiber, especially rice, to more refined carbohydrates such as sugar. The sugar intake of Thais has become an interesting issue owing to the information that the amount of intake has increased nearly threefold within only 30 years and the present consumption has been found to begin excess of the recommended level by the Thai Recommended Daily Intakes (Thai RDI) by four times (Food and Agriculture Organization, 2017).
Along with the changes in dietary pattern of the Thai population, Thailand has reached an important point in nutritional and health transition. Overnutrition, together with a reduction in physical activities, especially in activities associated with occupation and commuting among the population, has driven the prevalence of being overweight and obesity in Thailand. A report from the National Health Examination Survey showed that the percent of overweight and obese Thai adults with age 15 years and over increased dramatically from 20.4% in 1991 to nearly 50% in 2009 (Aekplakorn et al., 2014). This occurrence has not only happened in adults but has also grown continuously among Thai children. In 2009, the proportion of being overweight obesity in pre-school children and primary-school children aged between 6 and 14 years were 8.5% and 9.7% respectively (Chavasit, Kasemsup, & Tontisirin, 2013).
Aside from obesity, overnutrition has resulted in many diet-related chronic diseases such as diabetes, cardiovascular disease, hypertension, stroke and cancer (World Health Organization 2006) It is one of the main contributors to the burden of chronic diseases and disability of Thais and reduces the overall quality of Thai population’s life.The rapid emergence of obesity and other diet-related diseases have become increasingly important public health priorities (Aekplakorn et al., 2007; Wilbulpolprasert, 2008).This occurrence can lead to large health care costs both in developed nations and developing countries. The WHO has estimated that overnutrition accounted for 2-6% of total health care costs in several countries. The total cost attributable to obesity in Thailand was estimated at proximately 12,142 million baht which accounted for 0.13% of Thailand’s Gross Domestic Product (GDP)(Pitayatienanan et al., 2014).
The nutrition transition in Thailand has become an important concern for better health. Nowadays, energy dense, processed and Westernized foods are widely available and affordable throughout the country to all socio-economic consumer groups through the agency of transnational food company investments. However, higher income and more educated consumers are beginning to demand for more diverse and healthier diets just like the situation in more developed countries. The challenges for the Thai government and public health officials are to provide effective nutrition education and to boost affordable healthy diets for their population together with avoidance of the socio-economic inequity of nutritional outcome as observed in many rich nations(Kelly et al., 2010).
TRANSITION IN DIETARY PATTERNS AND NUTRITION STATUS
Similar to other countries in the Asia and Pacific region, Thailand has encountered socio-demographic and economic transitions. During this era, industry and services have replaced agriculture as the main sector of Thai economy. The social structure of Thais has also changed from a rural orientation to an urbanized society which creates changes in family and population ageing structures. The upward trend of small families has been observed and the population has changed from a mainly young population to an increased proportion of adults and the elderly (Kosulwat, 2002).
Rapid socio-economic transition together with the introduction of urbanization and Westernization has also influenced the lifestyles of the Thai population, particularly their dietary patterns. Previously, traditional Thai cuisine mainly consisted of rice and fish; while other types of meat were rarely included in any dishes. Basic ingredients such as fresh spices and herbs were commonly added to most Thai dishes. For a typical Thai meal, there are no “courses” instead; the dishes are served at the same time to complement each other. All side dishes are eaten with rice, which is the Thai main staple. During the transition period, eating patterns in Thailand have shifted from traditional Asian food with high cereal and low fat content towards Western diets consisting of a high proportion of meat, fats and sugar as similarity to transition in many Asian countries (B.M. Popkin, 2002; Barry M Popkin, 2004).
The transition of food consumption pattern in Thailand is demonstrated in Table 1. This table indicates the growth of meat, fish, dairy products and sugar consumption between 1975 and 2010. As a consequence of more animal product consumption, fat intake of Thais from animal sources has nearly doubled. Thai population has consumed dairy products including milk increasingly from only 19 grams/day in 1975 to 72 grams/day in 2010; whereas, the overall consumption of cereal and rice declined. People have moved from eating whole grain cereals and fiber, especially rice, to more refined carbohydrates such as sugar. Sugar intake emerges as an interesting issue for the current situation because the amount of intake has increased nearly threefold within only 30 years. In 2010, the daily sugar intake of Thais was up to 107.67 grams that was in excess of the recommended Thai RDI level (24 grams per day for added sugars) by nearly five times.
Table 1. Changes in food consumption in Thailand from 1975 to 2010
Unit: quantity/day/capita (g)
Year
Food item
1975
1985
1995
2005
2010
Rice & cereals
439.18
348.22
337.81
388.77
374.25
Rice
435.07
322.19
304.38
322.19
315.34
Vegetables
146.85
113.42
122.19
133.70
135.89
Fruits
246.58
258.63
255.62
318.63
292.33
Sugar & sweeteners
33.97
38.63
74.79
88.22
107.67
Meats
47.67
58.90
76.71
76.16
76.99
Fish & seafood
55.07
55.07
85.48
91.78
65.48
Milk
18.90
25.21
70.68
70.14
72.05
Fat from animal source
12.03
16.12
21.44
21.61
24.72
Fat from plant source
3.56
8.49
15.07
17.81
20.82
Source: Food and Agriculture Organization (2017)
It is not surprising that the energy consumption patterns of the Thai population have also changed during the transition period. Table 2 demonstrated the change in calorie and macronutrient intakes of Thai consumers from 1970 to 2010. The overall daily energy intake of Thais increased by approximately 590 kcal between 1980 and 2010 although it dropped down a little bit previously. An examination of macronutrient composition indicates that energy consumption from staple foods (carbohydrates) was replaced by calories from protein and fats. Thai consumers had the share of energy from protein around 9% of total energy. At the same time, the share of energy from fat in Thailand was nearly doubled and was supposed to grow continuously.
Table 2. Trends in dietary intake of energy, protein, fat and carbohydrate in Thailand from 1975 to 2010
Unit: kcal/day/capita
Year
1970
1980
1990
2000
2010
Energy (kcal)
2190
2170
2180
2604
2756
Protein (kcal)
205.72
193.52
196.92
237.76
236.40
As percentage of energy
9.39
8.92
9.03
9.13
8.58
Fat (kcal)
262.17
283.41
409.95
493.11
534.87
As percentage of energy
11.97
13.06
18.81
18.94
19.41
Carbohydrate (kcal)
1722.11
1693.07
1573.13
1873.13
1984.73
As percentage of energy
78.64
78.02
72.16
71.93
72.01
Source: (Food and Agriculture Organization (2017))
Most developing countries have undergone major socio-economic transition in the past three decades and now, they are approaching the post-transitional era. One worrying trend that has emerged during the transition is the “double burden” of malnutrition. Wherein undernutrition in some parts of the population co-exists with overnutrition and obesity in other segments(B.M. Popkin, Paeratakul, & Ge, 1995). Before the era of transition, the developing world had a high prevalence of undernutrition but socio-economic development together with the influences of urbanization and Westernization have shifted both the dietary and activity patterns of population, creating an upward trend in the incidence of obesity. Interestingly, this “double burden” exists not only at the country level but also at the household level(Kapoor & Anand, 2002).
The double burden of malnutrition during the nutrition transition has likely been related to the transition of epidemiology because overnutrition leads people to encounter non-communicable and degenerative diseases, while undernutrition has been associated with communicable diseases and reduction of productivity. The WHO noted that overnutrition and obesity are the major contributors to diet-related chronic diseases such as diabetes, cardiovascular disease, hypertension, stroke and cancer(World Health Organization 2006). Nowadays, stroke, heart disease and diabetes are among the top causes of mortality in Thailand (Porapakkham et al., 2010). Dietary risks are indicated as the important key factor of Disability-Adjusted Life Years (DAILs) lost for Thai population.
The trend of becoming overweight and obesity of Thai adults between 1991 and 2009 is shown in Fig. 1. This figure demonstrates that the prevalence of being overweight and obesity among Thai adults aged 15 years and over increased dramatically. The number of Thai adults who was overweight or had BMI ≥ 25 kg/m2has increased by 17.5% in 2009 compared to 1991. In 2009, the rate of obese adults having BMI ≥ 30 g/m2was 9.1%. It means that nearly 1 in 10 adults in Thailand have a tendency to face the obesity epidemic. As classified by gender, Thai females had a higher rate of being overweight and obese than males did over the period but the growth rate of this prevalence in males was up to 2.5 times while in females was double. In 2009, nearly half of Thai female adults tended to have their BMI larger than 25 g/m2 (Fig. 2)
Fig. 1. The prevalence of overweight and obesity of Thai adults between 1991 and 2009
Source:ThaiHealth (2014)
Fig. 2. The percentages of male and female Thai adults with BMI ≥ 25 kg/m2from 1991 to 2009
Source:ThaiHealth (2014)
FOOD CONSUMPTION TRENDS IN THAILAND
The linkage between food consumption and nutritional status of consumers is complex. Increased food consumption does not necessarily translate into better health and nutritional status. One of the important indicators of food security at either national or household levels is household food expenditure. A lower share of food expenditure in total spending can indicate better food security of households; however, the patterns of food expenditure in different food categories are needed to gain insights into changes in nutrition. The common factors affecting household or individual food consumption are: food prices; household income; food habits; cultural food beliefs; nutritional knowledge; food industry marketing and advertisements; tastes and preferences.
In Thailand, changes in socio-demographic patterns such as the increase in smaller sized households, increase in the female labor force, Westernization and urbanization have shifted consumers from having Thai staples with side dishes to consumption of foods with higher fats, animal meats, and less vegetables and fruits. The possible reason is that traditional Thai food requires lots of preparation time and many ingredients for cooking. Currently, Thai people tend to select food that needs less time and skill to prepare, so homemade meals, which were commonly seen in the past, have been replaced by ready-to-cook/eat foods and food away from home.
Food expenditure pattern of Thai households is showed in Table 3.This table indicates that average household size in Thailand became smaller during the period 1990 to 2010.Although the main share of food expenditure came from food at home, the share on this category decreased dramatically. At the same time, the overall expenditure on ready-to-eat food and food away from home rose over the period. The share on these two categories together increased from 24% to 46% within 24 years. An interesting point is the shaped growth of the share on ready to eat food of Thai households. Although the share on this category was only 8.8% of total food expenditure in 1990, Thai households tended to spend more on this category over the period. In 2014, the expenditure on this food group accounted about 21% of total food expenditure as well as it had a tendency to be nearby the share on food away from home category. In line with global market, convenient and ready to eat processed food products will become increasingly popular in Thailand due to lifestyle changes.
Table 3. Average expenditures spent on food prepared at home, prepared food taken home and food eaten away from home between 1990 and 2014inThailand (Nominal values)
Unit: Baht /month/ household
Type
Year
1990
1994
1998
2002
2006
2010
2014
Food prepared at home
1,494
1,881
2,609
2,397
2,491
3,056
3,491
%
(75.95)
(72.82)
(70.88)
(65.37)
(59.24)
(58.53)
(54.46)
Prepared food taken home
173
251
397
506
611
917
1,308
%
(8.80)
(9.72)
(10.79)
(13.82)
(14.53)
(17.56)
(20.41)
Food eaten away from home
300
451
675
763
1,103
1,248
1,610
%
(15.25)
(17.46)
(18.33)
(20.81)
(26.23)
(23.91)
(25.13)
No. of members in households
4.1
3.8
3.7
3.5
3.4
3.3
3.1
Note: Numbers in parentheses are the percentages of total food expenditure.
Source: Report of household socio-economic survey, 1990-2014
Owing to the prevalence of excessive sugar consumption, public health authorities in both developed and developing countries have investigated the patterns and trends in sugar consumption in their populations. One of the issues raised is about the largest sources of sugar in diets. Interestingly, the main source of added sugar in diets is not from eating desserts or consumption of raw sugar, but from the consumption of sugar sweetened beverages. Data from the National Cancer Institute in the United States indicates that nearly half of American sugar consumption comes from sugar-sweetened beverages with 36% from carbonated and functional drinks and 11% from fruit juices. Other sources of added sugar intake such as desserts and raw sugar account for only 19% and 3% respectively of total sugar intake. As in the US, a previous research conducted in Thailand showed that 60% of sugar consumption of Thai students resulted from drinking beverages with added sugars. The amount of sugar consumed from sugar-sweetened beverages was three and four times, respectively of that consumed from bakery items and Thai sweets- the second and third most important sources of sugar in Thai diets (Fig. 3).
Fig. 3. Sources of added sugar diets in U.S.A. and in Thailand
Note : a Data are drawn from “Sources of added sugars in the diets of the U.S. population ages 2 years and older”, NHANES 2005–2006 conducted by National Cancer Institute (2006)
bData are drawn from “Sucrose consumption in Thai undergraduate students” by Promdee, Trakulthong, and Kangwantrakul (2007)
The change in expenditure on sugar-sweetened beverages in Thailand is also captured in this paper. Table 4 presents the expenditure on non-alcoholic beverages of Thai households, which mostly consists of beverages with added sugars. This increased by four times during 16 years and the expenditure share for this item as compared to total food expenditure increased continuously over time. Euromonitor indicates that the consumption of non-alcoholic beverages mostly composed of beverages with added sugars has also risen and is expected to grow continuously until 2014(Euromonitor International, 2010).
Table 4. Averages expenditure and shares for non-alcoholic beverages between 1998 and 2014
Unit: Baht /month/ household
year
1998
2002
2006
2010
2014
Monthly household expenditure for
78.98
98.50
236.31
244
318
non-alcoholic beverages
Share for non-alcoholic beverages (%)
0.88
1.03
1.60
1.64
1.73
No. of members in households
3.7
3.5
3.4
3.3
3.1
Source: Calculated from Socio-Economic Surveys, 1998-2014
More than 80 % of Thai consumers today have access to supermarkets. The growth in access might be the result of urban movement of the population and increasing supermarket presence in non- urban areas. The association between frequent supermarket shopping and consumer group with urban residence and higher income is present in Thailand. Moreover, frequent shopping at supermarkets and convenience stores tends to be involved with the consumption of six “problem foods” (sugar-sweetened beverages, snacks, processed meats, Western style bakery products, instant foods and deep fried foods)(Kelly, Seubsman, Banwell, Dixon, & Sleigh, 2014). These foods commonly are energy dense and consist of high fat, sugar and salt that are associated with adverse impacts on health. In the same way, the WHO notes that the problem of being overweight and obesity is due to the fast change in lifestyle leading to the upward trend of eating out, eating ready to eat food cooked from local markets and food hawkers, and drinking soft drinks with high amounts of sugars. These foods are often low in nutritional value, but calorie dense and can cause overnutrition(World Health Organization, 2007).
However, the role of modern retail also has a positive impact on diets. The globalized food chains increase the diversity of food products available to consumers which induce to the potential for improvements in diet of population. The process of divergence of diets leads Thai consumers to begin a demand for more healthy foods (Kelly et al., 2010). The growing awareness of the healthy lifestyle results in an increasing demand for food items which not only provide basic nutrition but also support health. The report from THAILAND BOARD OF INVESTMENT (2013)indicates that Thai domestic market has strong demand for healthy food products. In 2011, Thai consumers spent around US$1.7 billion (or 56.5 billion baht) on health foods including sport nutrition, vitamin and dietary supplements, weight management, herbal products and allergy care foods. Even in snacks, there is an increase of health and wellness snacks. Many manufacturers have tried to reformulate their products reducing the amount of salt, sugar and fat in their products to respond the upward demand from Thai consumers for healthier snacks.
POLICY INTERVENTIONS TO PROMOTE HEALTHIER DIETS
Unhealthy dietary pattern of population can result in many diet-related chronic diseases such as diabetes, cardiovascular disease, hypertension, stroke, cancer and obesity. It can translate into a bigger burden for the government particularly in terms of large health care cost, lower quality of life and lost production. Policy interventions which are better suited can improve diets of population. Nutritional labeling which allows for informed choice is applied as one way to address the problem of unhealthy consumption in Thailand. In 2016, the Thai Ministry of public health issued a new regulation regarding food nutritional labeling to provide guidance of important nutritional information with Guideline Daily Amount (GDA)(Dachprasat, 2016). The GDA is a guideline for labeling the total amount of energy intake and some important nutrients (quantity of fat, sugar and sodium (or salt)) that may raise the risk of developing some diet-related diseases on the front of product package The GDA labeling is expected to help consumers on planning a healthy balanced consumption. It is believed that the nutritional knowledge related to consumer’s need and easy to understand is an essential factor to help consumer make an appropriate decision and help empowering them with the informed choice to have a balance diet. Example of GDA labeling on food product packages according to the notification is shown in Fig. 4.
Fig. 4. Example of GDA labelling on food product packages according to the notification
Source: Thailand Publishes New Regulation For Guideline Daily Amount (GDA) Labeling by (Dachprasat (2016))
However, informed choice does not necessarily bring about consumption of healthier foods although consumers know and are able to read and interpret nutritional labeling on food purchased. Interventions targeting the market environment such as fiscal measures might be generally more effective even though it is more intrusive (Brambila-Macias et al., 2011). Recently, Thai government introduced a tax on sugar-sweetened beverages because it is believed that consumers will cut back on consuming these product items and this method can reduce the health risks such as obesity and diabetes. Under the NRSA’s proposal, the retail price of this category will be increased by 20% to 25% (Bhadrakom, 2016). However, my previous research demonstrates that the higher price might not reduce excessive drinking of sugar-sweetened beverages due to the evidence of “habit formation” driving the consumption of these products in Thailand (Bhadrakom, 2014).
According to my study (Bhadrakom, 2014), the proposed tax on sugar-sweetened beverages would lead to only modest reductions in sugar consumption around 2.12 to 2.56 g/day in the case of adults and 3.61 to 4.36 g/day in the case of children. The larger values of long-run price elasticities in relation to short-run elasticities suggest that government revenues from the proposed tax would be lower over the long run. The tax would, however, not be regressive in terms of impact on lower income categories. Therefore, changing a formulated dietary habit takes time and requires other supportive measures. Fiscal measures will need to be supplemented by nutrition education, particularly for the younger age groups, to produce a significant reduction in unhealthy food consumption.
CONCLUSION
This article has reviewed the transition in dietary patterns and nutrition status in Thailand as a result of economic development and rapid urbanization during the past decades. The transition has been associated with significant shifts in dietary intake of Thai population characterized by an increase in fats, energy dense food and excessive sugar. The socio-economic transition has led Thai consumers to encounter non-communicable and diet-related chronic diseases such as diabetes, cardiovascular disease, stroke, cancers and obesity.
Furthermore, this article has also reviewed the trend of food consumption in Thailand. We found that Thai people tend to select food which needs less time and skill to prepare. Therefore, food expenditure of Thai households on food prepared at home has been replaced by ready-to-cook/eat foods and food away from home. The excessive sugar consumption of Thais is also raised as an important issue for public health today. Previous papers report that the main source of added sugar in diet is from drinking sugar-sweetened beverages. Compared to total food expenditure, Thai households tend to spend more on this category continuously over time. Moreover, the role of modern retail gives an impact on food consumption pattern of Thai population. Frequent shopping at supermarket and convenience stores is involved with the consumption of six “problem foods” (sugar-sweetened beverages, snacks, processed meats, western style bakery products, instant foods and deep fried foods). On the other hand, the globalized food chains increase the diversity of food products available to consumers to potential for improvements in their diet. Nowadays, some parts of Thai consumers begin a demand for healthy foods and they have a growing awareness of the healthy lifestyle.
For the final point, we have talked about the policy interventions to promote healthier diets in Thailand. Recently, Thai government issued a new regulation regarding food nutritional labeling with GDA and fiscal measure as a tax on sugar-sweetened beverages. These measures are believed to reduce the consumption of unhealthy foods and cut health risks from diet-related chronic diseases. However, the measures will need to be supplemented by nutrition education particularly for the young children because food habits in early stages of life determine practices and preferences in adulthood. The consumption at schools needs to be addressed for example reduction in students’ access to sugar-sweetened beverages and unhealthy snacks. Moreover, another challenge of Thai government is to boost affordable healthy diets for their population and reduce the socio-economic inequity of nutritional outcomes due to cost constraints in poorer consumers.
REFERENCES
Aekplakorn, W. (2010). National health examination survey IV report 2008-2009. Thailand: The Graphico system co, Ltd.
Aekplakorn, W., Hogan, M. C., Chongsuvivatwong, V., Tatsanavivat, P., Chariyalertsak, S., Boonthum, A., . . . Lim, S. S. (2007). Trends in Obesity and Associations with Education and Urban or Rural Residence in Thailand. OBESITY 15(2), 3113-3121.
Aekplakorn, W., Inthawong, R., Kessomboon, P., Sangthong, R., Chariyalertsak, S., Putwatana, P., & Taneepanichskul, S. (2014). Prevalence and trends of obesity and association with socioeconomic status in Thai adults: national health examination surveys, 1991–2009. Journal of obesity, 2014.
Bhadrakom, C. (2014). Economic analysis of overnutrition in Thailand. University of Reading.
Bhadrakom, C. (2016, 15 Jun 2016). A sugar tax is not the answer to obesity Bangkok Post. Retrieved from https://www.bangkokpost.com/opinion/opinion/1010545/a-sugar-tax-is-not-t...
Brambila-Macias, J., Shankar, B., Capacci, S., Mazzocchi, M., Perez-Cueto, F. J. A., Verbeke, W., & Traill, W. B. (2011). Policy Interventions to Promote Healthy Eating: A Review of What Works, What Does Not, and What is Promising. Food and Nutrition Bulletin, 32(4), 365-375. doi: 10.1177/156482651103200408
Chavasit, V., Kasemsup, V., & Tontisirin, K. (2013). Thailand conquered under‐nutrition very successfully but has not slowed obesity. Obesity reviews, 14(S2), 96-105.
Dachprasat, N. (2016). Thailand Publishes New Regulation For Guideline Daily Amount (GDA) Labeling from www.foodsafety.sgs.com
Euromonitor International. (2010). Non-alcohol beverages in Thailand. Retrieved Aug, 11, 2012, from http://www.portal.euromonitor.com/portal/default.aspx
Food and Agriculture Organization. (2017). FAO Food Balance Sheets. Retrieved 10/6/2018, from United Nations
Kapoor, S., & Anand, K. (2002). Nutritional transition: a public health challenge in developing countries. Journal of epidemiology and community health, 56(11), 804-805.
Kelly, M., Banwell, C., Dixon, J., Seubsman, S.-a., Yiengprugsawan, V., & Sleigh, A. (2010). Nutrition transition, food retailing and health equity in Thailand. Australasian epidemiologist/Australasian Epidemiological Association, 17(3), 4.
Kelly, M., Seubsman, S.-a., Banwell, C., Dixon, J., & Sleigh, A. (2014). Thailand's food retail transition: supermarket and fresh market effects on diet quality and health. British Food Journal, 116(7), 1180-1193.
Kosulwat, V. (2002). The Nutrition and Health Transition in Thailand. Public Health Nutr., 5, 183-189.
National Cancer Institute. (2006). Sources of added sugars in the diets of the U.S. population ages 2 years and older,NHANES 2005–2006. Risk Factor Monitoring and Methods. Cancer Control and Population Sciences. . Retrieved August 11, 2012, from http://riskfactor.cancer.gov/diet/foodsources/added_sugars/table5a.html.
Pitayatienanan, P., Butchon, R., Yothasamut, J., Aekplakorn, W., Teerawattananon, Y., Suksomboon, N., & Thavorncharoensap, M. (2014). Economic costs of obesity in Thailand: a retrospective cost-of-illness study. BMC health services research, 14(1), 146.
Popkin, B. M. (2002). An overview on the nutrition transition and its health implications: the Bellagio meeting. Public health nutrition, 5(1A), 93.
Popkin, B. M. (2004). The nutrition transition and the global shift towards obesity. Diabetes in Society, 49(3).
Popkin, B. M., Paeratakul, S., & Ge, K. (1995). A review of dietary and environmental correlates of obesity with emphasis on developing countries. Obesity Research, 3, 145-153.
Porapakkham, Y., Rao, C., Pattaraarchachai, J., Polprasert, W., Vos, T., Adair, T., & Lopez, A. D. (2010). Estimated causes of death in Thailand, 2005: implications for health policy. Population Health Metrics, 8(1), 14.
Promdee, L., Trakulthong, J., & Kangwantrakul, W. (2007). Sucrose consumption in Thai undergraduate students. Asia Pac J Clin Nutr, 16(Suppl 1), 22-26.
ThaiHealth. (2014). "Self-management Communities:" Foundation of National Reform. Nakhon Pathom , Thailand: Institute for Population and Social Research , Mahidol University.
THAILAND BOARD OF INVESTMENT. (2013). Thailand’s Food Industry: THAILAND BOARD OF INVESTMENT.
Wilbulpolprasert, S. (2008). Thailand Health Profile 2005–2007. Bangkok: Ministry of Public Health.
World Health Organization (2006). Obesity and Overweight. Retrieved June 10, 2010, from http://www.who.int/mediacentre/factsheets/fs311/en/print.html
World Health Organization. (2007). Thailand National Health System Profile 2007. Retrieved March 12, 2012, from http://www.searo.who.int/LinkFiles/Thailand_Thailand_final_031005_WT.pdf
Date submitted: July 11, 2018
Reviewed, edited and uploaded: Sept. 10, 2018